Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Selinexor combined bortezomib, lenalidomide, and dexamethasone for newly diagnosed multiple myeloma with high-risk cytogenetics abnormalities: A single-arm, multi-center, observational clinical study
(PA-461) Selinexor Combined Bortezomib, Lenalidomide, and Dexamethasone for Newly Diagnosed Multiple Myeloma with High-risk Cytogenetics Abnormalities: A Single-arm, Multi-center, Observational Clinical Study

Yuping Zhong, Doctor
Physician
University of Health and Rehabilitation Science&Qingdao Municipal Hospital
Over the past 20 years, survival of multiple myeloma (MM) has significantly improved,however certain cytogenetic abnormalities are associated with poor prognosis. Cytogenetic abnormalities are the core indicators in the risk stratification system of MM. To date, no standardized treatment approach for NDMM with high risk (HR)CAs. Selinexor(X) is a first-in-class Selective Inhibitor of Nuclear Export (SINE) small molecule compound that selectively binds and inactivates XPO1.Previous studies have demonstrated its clinical activity in patients with HRCAs.
Methods:
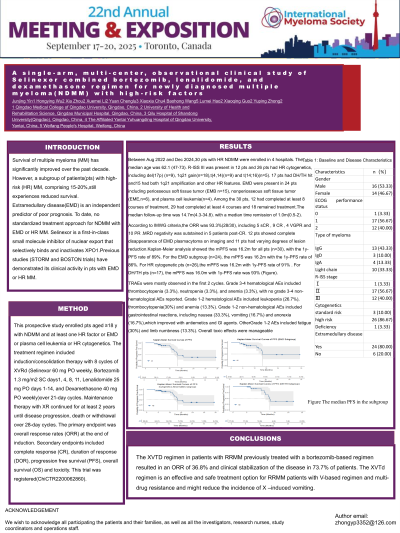
This prospective study enrolled patients aged ≥18 with NDMM and at least 1 HRCAs. The treatment regimen is induction/consolidation therapy with 8 cycles of XVRd (X 60 mg PO weekly, bortezomib 1.3 mg/m2 SC days1, 4, 8, 11, Lenalidomide 25 mg PO days 1-14, and Dexamethasone 40 mg PO weekly)over 21-day cycles. Maintenance therapy with XR continued for at least 2 years until disease progression, death or withdrawal over 28-day cycles. The primary endpoint was overall response rates (ORR) at the end of induction. Secondary endpoints included complete response (CR), duration of response (DOR), progression free survival (PFS), overall survival (OS) and toxicity.
This trial was registered ChiCTR2200062860.
Results:
Between August 2022 to December 2024, 26 pts with NDMM and at least one CAs were enrolled in 4 hospitals. The median age was 61.5 (R 47-73). R-ISS stage III was present in 11 pts, CAs are including del(17p) (n=9), 1q21 gain(n=18),t(4,14)(n=9) and t(14;16)(n=5). 17 pts had double-hit or triple-hit and 15 had both 1q21 amplification and others.Among the 26 pts, 10 had completed at least 8 courses of treatment, 25 at least 4 courses and 18 remained treatment. The median follow-up time was 15.7 months(range 4.3-34.8). with a median time remission of 1 month(range 0.5-2) .According to IMWG criteria,the ORR was 92.3%, including 5 sCR , 9 CR , 4 VGPR and 10 PR, MRD negativity was sutstained in 5 pts after achieving CR. For CAs pts (n = 26), the m PFS was 16.2 months (95%CI: 14.6-NA) with a 1-y PFS rate of 91% (95%CI: 0.8-1). For CAs pts with DH/TH (n = 17), the mPFS was 16 months (95%CI: 14.1-NA) with a 1-y PFS rate was 93% (95%CI: 0.8-1). TRAEs were mostly observed in the first 2 cycles. Grade 3-4 hematological AEs included thrombocytopenia (3.3%), neutropenia (3.3%), and anemia (3.3%). Grade 1-2 hematological AEs included leukopenia (26.7%), thrombocytopenia(30%) and anemia (13.3%). Grade 1-2 non-hematological AEs included including nausea (33.3%), vomiting (16.7%) and anorexia (16.7%),which improved with antiemetics and GI agents. Other Grade 1-2 AEs are fatigue (30%) and limb numbness (13.3%). Overall toxic effects were manageable.
Conclusions:
The XVRd regimen as induction therapy prior to ASCT is safe and effective in achieving deep responses in NDMM pts with CAs. These preliminary results warrant further investigation. Long-term outcomes will be assessed as more patients are enrolled and followed up.
