Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
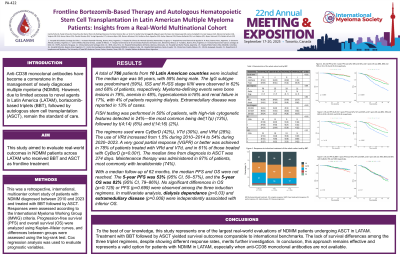
Frontline Bortezomib-Based Therapy and Autologous Hematopoietic Stem Cell Transplantation in Latin American Multiple Myeloma Patients: Insights from a Real-World Multinational Cohort
(PA-422) Frontline Bortezomib-Based Therapy and Autologous Hematopoietic Stem Cell Transplantation in Latin American Multiple Myeloma Patients: Insights from a Real-World Multinational Cohort

Camila Peña, MD (she/her/hers)
Hematologist
Hospital del Salvador
Introduction:
Anti-CD38 monoclonal antibodies have become a cornerstone in the management of newly diagnosed multiple myeloma (NDMM). However, due to limited access to novel agents in Latin America (LATAM), bortezomib-based triplets (BBT), followed by autologous stem cell transplantation (ASCT), remain the standard of care. This study aimed to evaluate real-world outcomes in NDMM patients across LATAM who received BBT and ASCT as frontline treatment.
Methods:
This was a retrospective, international, multicenter cohort study of patients with NDMM diagnosed between 2010 and 2023 and treated with BBT followed by ASCT. Responses were assessed according to the International Myeloma Working Group (IMWG) criteria. Progression-free survival (PFS) and overall survival (OS) were analyzed using Kaplan–Meier curves, and differences between groups were assessed using the log-rank test. Cox regression analysis was used to evaluate prognostic variables.
Results:
A total of 766 patients from 10 Latin American countries were included. The median age was 56 years, with 59% being male. The IgG subtype was predominant (59%). ISS and R-ISS stage II/III were observed in 62% and 68% of patients, respectively. The most common myeloma-defining events were bone lesions (79%), anemia (48%), hypercalcemia (18%) and renal failure (17%). Extramedullary disease was reported in 13% of cases.
FISH testing was performed in 50% of patients, with high-risk cytogenetic features detected in 24%—the most common being del(17p) (13%), followed by t(4;14) (6%) and t(14;16) (2%).
The regimens used were CyBorD (42%), VTd (30%), and VRd (28%). The use of VRd increased from 1.5% during 2010–2014 to 54% during 2020–2023. A very good partial response (VGPR) or better was achieved in 78% of patients treated with VRd and VTd, and in 61% of those treated with CyBorD (p< 0.001). The median time from diagnosis to ASCT was 274 days. Maintenance therapy was administered in 87% of patients, most commonly with lenalidomide (74%).
With a median follow-up of 62 months, the median PFS and OS were not reached. The 5-year PFS was 53% (95% CI, 50–57%), and the 5-year OS was 82% (95% CI, 79–86%). No significant differences in OS (p=0.125) or PFS (p=0.699) were observed among the three induction regimens. In multivariate analysis, dialysis dependance (p=0.03) and extramedullary disease (p=0.008) were independently associated with inferior OS.
Conclusions:
To the best of our knowledge, this study represents one of the largest real-world evaluations of NDMM patients undergoing ASCT in LATAM. Treatment with BBT followed by ASCT yielded survival outcomes comparable to international benchmarks. The lack of survival differences among the three triplet regimens, despite showing different response rates, merits further investigation. In conclusion, this approach remains effective and represents a valid option for patients with NDMM in LATAM, especially when anti-CD38 monoclonal antibodies are not available.
