Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Characteristics and outcomes of Multiple Myeloma patients with post-transplant relapse: A Latin American Real-World Cohort Study
(PA-501) Characteristics and Outcomes of Multiple Myeloma Patients with Post-transplant Relapse: A Latin American Real-world Cohort Study

Camila Peña, MD (she/her/hers)
Hematologist
Hospital del Salvador
Introduction:
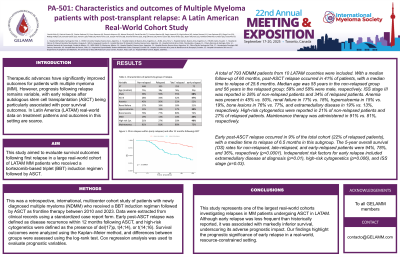
Therapeutic advances have significantly improved outcomes for patients with multiple myeloma (MM). However, prognosis following relapse remains variable, with early relapse after autologous stem cell transplantation (ASCT) being particularly associated with poor survival outcomes. In Latin America (LATAM), access to novel therapies for relapsed/refractory multiple myeloma (RRMM) remains limited, and real-world data on treatment patterns and outcomes in this setting are scarce.
This study aimed to evaluate survival outcomes following first relapse in a large real-world cohort of LATAM MM patients who received a bortezomib-based triplet (BBT) induction regimen followed by ASCT.
Methods:
This was a retrospective, international, multicenter cohort study of patients with newly diagnosed multiple myeloma (NDMM) who received a BBT induction regimen followed by ASCT as frontline therapy between 2010 and 2023. Data were extracted from clinical records using a standardized case report form. Early post-ASCT relapse was defined as disease recurrence within 12 months following ASCT, and high-risk cytogenetics were defined as the presence of del(17)p, t(4;14), or t(14;16). Survival outcomes were analyzed using the Kaplan–Meier method, and differences between groups were assessed using the log-rank test. Cox regression analysis was used to evaluate prognostic variables.
Results:
A total of 793 NDMM patients from 10 LATAM countries were included. With a median follow-up of 60 months, post-ASCT relapse occurred in 41% of patients, with a median time to relapse of 25.6 months. Median age was 55 years in the non-relapsed group and 56 years in the relapsed group; 59% and 58% were male, respectively. ISS stage III was reported in 28% of non-relapsed patients and 34% of relapsed patients. Anemia was present in 45% vs. 50%, renal failure in 17% vs. 18%, hypercalcemia in 15% vs. 19%, bone lesions in 76% vs. 77%, and extramedullary disease in 19% vs. 13%, respectively. High-risk cytogenetics were reported in 21% of non-relapsed patients and 27% of relapsed patients. Maintenance therapy was administered in 91% vs. 81%, respectively.
Early post-ASCT relapse occurred in 10% of the total cohort (29% of relapsed patients), with a median time to relapse of 6.5 months in this subgroup. The 5-year overall survival (OS) rates for non-relapsed, late-relapsed, and early-relapsed patients were 94%, 78%, and 36%, respectively (p< 0.0001). Independent risk factors for early relapse included extramedullary disease at diagnosis (p=0.01), high-risk cytogenetics (p=0.006), and ISS stage (p=0.03).
Conclusions:
This study represents one of the largest real-world cohorts investigating relapse in NDMM patients undergoing ASCT in LATAM. Although early relapse was less frequent than historically reported, it was associated with markedly inferior survival, underscoring its adverse prognostic impact. Our findings highlight the prognostic significance of early relapse in a real-world, resource-constrained setting.
