MRD and Biomarkers
Category: MRD and Biomarkers
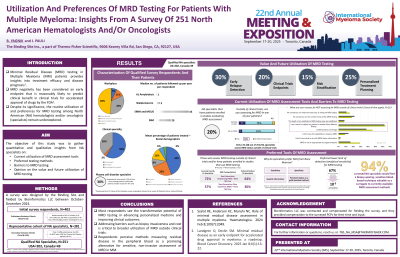
Utilization and Preferences of MRD Testing for patients with Multiple Myeloma: Insights from a Survey of 251 North American Hematologists and/or Oncologists
(PA-197) Utilization and Preferences of MRD Testing for Patients with Multiple Myeloma: Insights from a Survey of 251 North American Hematologists And/or Oncologists
.jpg)
Bhrugu Yagnik, M.S., PhD (he/him/his)
Medical Science Liaison (MSL)
The Binding Site, part of Thermo Fisher Scientific
Minimal Residual Disease (MRD) testing in Multiple Myeloma (MM) patients provides insights into treatment efficacy and disease prognosis. MRD negativity has been considered an early endpoint that is reasonably likely to predict clinical benefit in clinical trials for accelerated approval of drugs by the FDA. Despite its significance, the routine utilization of and preferences for MRD testing among North American (NA) hematologists and/or oncologists (specialists) remain underexplored.
Methods:
A comprehensive survey was designed to gather quantitative and qualitative insights about the current utilization of MRD assessment tools, preferred testing methods, barriers to MRD testing, and opinion on the value and potential future utilization of MRD testing from NA specialists. Eligible specialists must have practiced either in the US or Canada and must have treated at least 5 or more MM patients per year. A life science market research company fielded this survey between October – December 2024, including responses from 202 US and 49 Canadian specialists.
Results:
Survey respondents perceive MRD testing as valuable for early relapse detection (~30%), clinical trials endpoints (~20%), risk stratification (~15%), and personalized treatment planning (~25%), which can improve patient outcomes. However, most specialists do not assess MRD status outside clinical trials, with only 11% (28 out of 251) of respondents actively doing so. The two key barriers to MRD utilization are the reluctance to subject patients to additional bone marrow biopsies (63%) and concerns about cost and insurance coverage (45%). Next-Generation Sequencing (NGS) in the bone marrow is both the most utilized and preferred method among the specialists who do utilize MRD for their myeloma patients (n=61). Common reasons for favoring NGS-bone marrow compared to other available methods include its sensitivity, specificity, genetic information, and its perceived status as the standard method. The lower limit of detection for 67% of NA specialists’ preferred MRD testing is 1 aberrant plasma cell in 10,000 cells (10−5). 94% of surveyed NA specialists would find a biopsy-sparing, sensitive blood-based technique valuable as a surrogate to currently available MRD assessment methods.
Conclusions:
Most respondents see the transformative potential of MRD testing in advancing personalized medicine and improving clinical outcomes. Addressing barriers such as biopsy invasiveness and cost is critical to broader utilization of MRD outside clinical trials. Respondents perceive methods measuring residual disease in the peripheral blood as a promising alternative for sensitive, non-invasive assessment of MRD in MM.
