Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
Outcomes of CAR-T Cell Therapy in patients with AL Amyloidosis
(PA-093) Outcomes of CAR-T Cell Therapy in patients with AL Amyloidosis

Melinda Tan, Dr
Fellow
Mayo Clinic
Introduction:
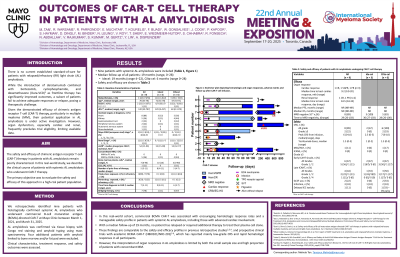
The safety and efficacy of chimeric antigen receptor T-cell (CAR-T) therapy in patients with AL amyloidosis remain poorly characterized. Given the challenges posed by amyloid-related organ dysfunction, we evaluated the clinical outcomes of CAR-T therapy in this high-risk population.
Methods: We retrospectively analyzed patients with biopsy-confirmed AL amyloidosis treated with CAR-T from March 2021 to April 2025. Clinical characteristics, treatment response, and safety outcomes were assessed.
Results:
Nine patients with systemic AL amyloidosis were included. Organ involvement included cardiac (8), renal (5), peripheral nerve (2), gastrointestinal (2), autonomic (1), and musculoskeletal (1). Five had single-organ, 4 had 2-organ, and 1 had 3-organ involvement. Five patients met CRAB criteria for concurrent multiple myeloma. Median age at infusion was 69 years (range 33–78). Six patients received ciltacabtagene autoleucel and 3 idecabtagene vicleucel. Patients had a median of 5 prior therapies (range 3–11), and 7 were triple-class refractory; none had prior T-cell redirecting therapies. At diagnosis, the Mayo 2004 with European modification stages were stage II (5), IIIa (3), and IIIb (1).
The median duration of severe neutropenia (ANC< 500/µl) within 30 days was 4 (range 0-9). Early immune effector cell-associated hematotoxicity (ICAHT) occurred in 7 patients (5 grade 1, 1 grade 2), and late ICAHT in 4 (2 grade 1, 1 grade 2, 1 grade 3). Rates were comparable to a reference cohort of 180 MM patients treated with CAR-T. Supportive measures included filgrastim (2) and romiplostim (1). Infections occurred in 3 patients, and HLH in 1 (with high marrow plasma cell burden).
CRS occurred in 8 of 9 patients, with 2 grade 3 events, and was more frequent than in MM patients (p < 0.01). All cases resolved with supportive management. One patient with cardiac amyloidosis developed supraventricular tachycardia that was medically managed. No cases of ICANS, clinically significant worsening of AL-related organ function, delayed neurotoxicity, colitis, or secondary malignancies were observed.
Eight patients were evaluable for hematologic response; all achieved complete response with a median time to best response of 31 days (range 26–138). Seven achieved minimal residual disease negativity at a median of 29 days (range 26–103). At a median follow-up of 19 months (range 4-20), none of the 3 ide-cel patients relapsed. Of three patients eligible for cardiac response assessment, one achieved partial, one very good partial, and one complete response, with a median time to best cardiac response of 9.2 months. None met criteria for renal response assessment. At a median follow-up of 18 months, no relapses or deaths were reported.
Conclusions:
CAR-T therapy in AL amyloidosis patients showed high response rates with manageable toxicities, despite prevalent cardiac involvement. These findings support the feasibility and therapeutic potential of CAR-T therapy in this understudied population.
