Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Health-related quality of life (HRQoL) in frail patients with newly diagnosed multiple myeloma (NDMM) treated with isatuximab (Isa), bortezomib, lenalidomide, and dexamethasone (Isa-VRd) vs VRd alone
(PA-379) Health-related Quality of Life (HRQoL) in Frail Patients with Newly Diagnosed Multiple Myeloma (NDMM) Treated with Isatuximab (Isa), Bortezomib, Lenalidomide, and Dexamethasone (Isa-VRd) vs VRd Alone

Robert Z. Orlowski, MD, PhD (he/him/his)
Professor
Department of Lymphoma and Myeloma, The University of Texas MD Anderson Cancer Center
Introduction:
NDMM patients (pts) who meet frailty criteria have worse outcomes vs non-frail pts. A post hoc analysis of the phase 3 IMROZ study (NCT03319667) demonstrated Isa-VRd significantly improved progression-free survival and achieved deep responses vs VRd in both frail and non-frail pts. This study investigated HRQoL in a subgroup of frail pts in IMROZ.
Methods:
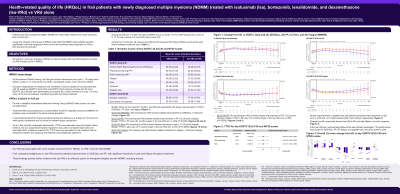
We analyzed patient-reported outcomes (PRO) in a subgroup of frail pts (frailty score ≥2 based on age, ECOG performance status, and comorbidities) as defined by the simplified International Myeloma Working Group (sIMWG). PRO instruments, including European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire with 30 questions (EORTC QLQ-C30); EORTC QLQ myeloma module with 20 items (EORTC QLQ-MY20); and European Quality of Life Group 5-dimension, 5-Level Questionnaire (EQ 5D 5L), were administered at baseline (BL), prior to treatment on Day 1 of every cycle, at the end of treatment, and 90±5 days after last study treatment. Meaningful thresholds for within- and between-group improvement/worsening were defined a priori based on published literature (≥10- and ≥5-point change, respectively). Treatment effect was assessed by a mixed-effects model for repeated measures. Time to first deterioration was estimated using the Kaplan Meier method and Cox proportional hazards regression was used to compute hazard ratio and associated 95% confidence interval (CI).
Results: Overall, 119/446 (26.7%) pts were classified as frail (69 [26.0%] Isa-VRd; 50 [27.6%] VRd). Median follow-up was 59.7 mo overall. In frail pts, Isa-VRd was associated with larger improvements vs VRd in GHS/QoL, pain, fatigue, and physical functioning, with a difference in LS mean change from BL (standard error) [95% CI; p-value] of 3.50 (3.24) [–2.92, 9.91; 0.2825]; –1.90 (4.60) [–11.00, 7.20; 0.6802]; –6.44 (3.90) [–14.16, 1.29; 0.1018]; and 10.67 (4.56) [1.65, 19.69; 0.0209], respectively. Frail pts receiving Isa-VRd showed notable reductions overall in pain (–17.92-point change), >20 points at multiple cycles, and fatigue (–8.48). Similar improvements in appetite loss and disease symptoms were observed in both treatment arms. Change from BL numerically favored Isa-VRd in other scales (role functioning, side effects), except for dyspnea. In frail pts, Isa-VRd vs VRd was associated with statistically longer median time to first clinically meaningful deterioration in physical functioning (6.93 vs 3.12 mo, p=0.0034), pain (6.93 vs 2.92 mo, p=0.0060) and role functioning (6.11 vs 2.60 mo, p=0.0032).
Conclusions:
Isa-VRd was associated with more durable improvements in HRQoL vs VRd in all pts with NDMM, including frail pts. Frail pts on Isa-VRd showed sustained improvements in GHS/QoL and physical function, with significant reductions in pain and fatigue throughout treatment. These findings provide further evidence that Isa-VRd is an effective option with a manageable safety profile for frail pts with NDMM.
