Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
Drivers of primary resistance to BCMA-targeted T cell redirected therapies in high tumor burden
(PA-084) Drivers of Primary Resistance to BCMA-targeted T Cell Redirected Therapies in High Tumor Burden

Kirsten Pfeffer, PhD
Research Fellow
Mayo Clinic
T cell engager (TCE) and CAR-T targeting BCMA have shown promising activity and efficacy in heavily pre-treated, relapsed/refractory multiple myeloma. Although deep responses can be achieved, most inevitably relapse. Patients with high tumor burden, or low effector-to-target ratio, are more resistant to these therapies. In addition to tumor debulking, novel strategies are needed to overcome primary resistance. We aimed to investigate in vitro and in vivo T cell intrinsic and extrinsic mechanisms of primary resistance in high tumor burden that mimics clinical conditions, using the immunocompetent Vk*MYC mouse model of MM. We tested three strategies to improve anti-BCMA mediated T cell activity: increasing TCE dose, increasing surface BCMA while reducing soluble BCMA with gamma-secretase inhibition (GSi), or boosting T cell function by combination with IMiDs.
Methods:
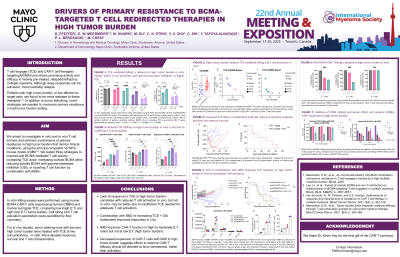
In vitro killing assays were performed using murine CAR-T cells (expressing human CRBN) and murine surrogate TCE, comparing low (high E:T) and high (low E:T) tumor burden. Cell killing and T cell activation parameters were quantified by flow cytometry. For in vivo studies, tumor bearing mice with low and high tumor burden were treated with TCE at two concentrations, -/+ GSi. We evaluated response, survival and T cell characteristics.
Results:
In vitro, we observed proportional decrease in TCE-mediated tumor killing as E:T ratio decreased (from 7:1 to 1:2), that was not associated with reduced T cell activation or imbalanced T cell:tumor proliferation. Adding GSi and increasing TCE was not sufficient to overcome high tumor burden. Reduced killing in vitro therefore results from tumor intrinsic mechanisms that require further exploration. Conversely, in vivo we found a proportional decrease in T cell activation as tumor burden increases, that was only transiently overcome by combination with IMiDs or by increased TCE + GSi, without improving OS. This suggests limited TCE engagement and highlights a more complex scenario in vivo that cannot be completely replicated in vitro. Regardless of tumor burden, CAR-T kill effectively at 72h, consistent with clinically observed high response rates. Though, earlier timepoints (24-48h) showed decreased function and expansion in high tumor burden. Surprisingly, at low E:T, POM inhibited CAR-T expansion and reduced antitumor effect, suggesting deleterious effects of hyperactivation.
Conclusions:
Lack of response to TCE in high tumor burden correlates with reduced T cell activation in vivo, but not in vitro, may be partly due to insufficient TCE needed for adequate T cell activation. Consistently, combination with IMiD or increasing TCE moderately improved responses, but only when combined with GSi. CAR-T activity is less dependent on tumor burden. Unexpectedly, IMiD did not improve CAR-T function and at low E:T lead to decreased expansion and functional exhaustion, suggesting efforts to improve CAR-T efficacy should be directed to favor persistence, rather than activation.
