Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
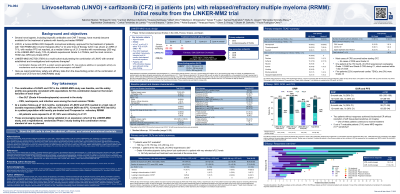
Linvoseltamab (LINVO) + carfilzomib (CFZ) in patients (pts) with relapsed/refractory multiple myeloma (RRMM): Initial results from the LINKER-MM2 trial
(PA-064) Linvoseltamab (LINVO) + Carfilzomib (CFZ) in Patients (pts) with Relapsed/refractory Multiple Myeloma (RRMM): Initial Results from the LINKER-MM2 Trial

Salomon Manier, MD, PhD
Associate Professor
Hematology Department, Lille University Hospital, Lille, France
LINVO, a human BCMA×CD3 bispecific antibody, demonstrated high efficacy and a generally manageable safety profile in pts with triple-class exposed (TCE) RRMM. Combination treatment (tx) with CFZ, a potent 2nd-generation proteasome inhibitor (PI), may provide additive or synergistic activity. We report safety and preliminary efficacy from the dose-finding portion in the LINVO + CFZ cohort of the Phase 1b LINKER-MM2 trial (NCT05137054).
Methods:
Eligible pts were aged ≥18 years with RRMM that progressed after ≥3 lines of therapy (LoT), or ≥2 LoT if TCE or double-class refractory (immunomodulatory drug + PI). Prior CFZ was allowed if previously tolerated and ≥6 months had elapsed since last exposure. CFZ-refractory pts were allowed during dose finding. Tx began with LINVO alone (Cycle [C] 0) as two step-up doses (5 mg, 25 mg) and three full doses (dose level [DL] 1: 100 mg; DL1b: 150 mg; DL2: 200 mg) before initiation of CFZ (20/56 mg/m2 on Days 1, 2, 8, 9, 15, 16) at C1. LINVO was given once weekly (QW) in C1–4, and once every 2 weeks thereafter. CFZ dosing could be switched to QW after C2. Dexamethasone premedication was given at C0–1. Primary endpoints were dose-limiting toxicities (DLTs) and tx-emergent adverse events (TEAEs). Secondary endpoints included objective response rate (ORR), duration of response (DOR), and progression-free survival (PFS).
Results:
As of 7 Mar, 2025, 23 pts were treated at DL1 (n=12), DL1b (n=6), or DL2 (n=5). All pts had received ≥1 PI and 52% were refractory to ≥1 PI. Median number of prior LoT was 3 (range 2–6), including 91% of pts with TCE and 43% with triple-class refractory disease. Median age was 70 years (range 53–83), 48% were male, 4% had ISS stage III at study entry, 17% had high-risk cytogenetics, and 22% had sBCMA ≥400 ng/mL. Median duration of follow-up was 22.3 (DL1), 13.2 (DL1b), and 5.6 months (DL2), with 42%, 83% and 80% of pts still receiving tx, respectively. The most common TEAEs were neutropenia (any Grade [Gr] 61%; Gr 3–4 52%), cytokine release syndrome (61%; 0%), thrombocytopenia (52%; 30%), and diarrhea (52%; 4%). One pt experienced ICANS (Gr 1). Infections were reported in 91% of pts (Gr ≥3 43%). One DLT was observed at DL1, Gr 4 thrombocytopenia during tumor lysis syndrome, which was fully resolved and tx resumed at the same dose. Among evaluable pts, ORR was 91% at DL1 (10/11; very good partial response or better [≥VGPR] rate 91%), 100% at DL1b (5/5; ≥VGPR rate 100%), and 80% at DL2 (3/5; ≥VGPR rate 60%); 5/7 minimal residual disease (MRD)-evaluable pts were MRD negative (10-5 threshold). DOR rate was 87% (95% CI 56–97) and PFS rate was 83% (95% CI 55–94) at 12 months.
Conclusions:
In pts with heavily pretreated RRMM and prior PI exposure, LINVO + CFZ induced a high rate of deep and durable responses with a safety profile generally consistent with that expected based on the individual drug profiles. These preliminary data support continued development of LINVO + CFZ for the tx of pts with heavily pre-treated RRMM.
