Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
Integrating real-world evidence to augment crossover adjustment in KarMMa-3: a case study in relapsed/refractory multiple myeloma
(PA-069) Integrating Real-world Evidence to Augment Crossover Adjustment in KarMMa-3: A Case Study in Relapsed/Refractory Multiple Myeloma
.jpg)
Paula Rodríguez-Otero, MD, PhD (she/her/hers)
Medical Coordinator
Cancer Center Clínica Universidad de Navarra, Centro de Investigación Médica Aplicada (CIMA), Instituto de Investigación Sanitaria de Navarra (IdiSNA)
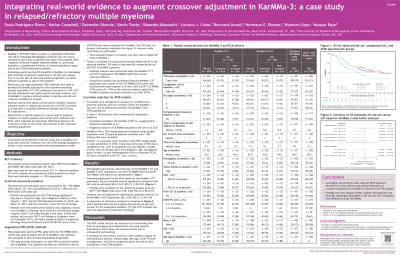
KarMMa-3 (NCT03651128) is a phase 3 randomized controlled trial evaluating idecabtagene vicleucel (ide-cel) versus standard of care (SoC) in patients with triple-class exposed (TCE) relapsed/refractory multiple myeloma (RRMM). Evaluating overall survival (OS) benefits in KarMMa-3 is challenging, given that 56% of patients randomized to the SoC arm crossed over to ide-cel following disease progression (unadjusted OS hazard ratio [HR], 1.01; 95% confidence interval [CI], 0.73–1.40). Two-stage estimation methods were used to estimate OS benefits adjusted for crossover (HR, 0.72; 95% CI, 0.49–1.01), but this adjustment was limited by the small number of patients who did not crossover. We aimed to estimate the OS benefit of ide-cel versus SoC in KarMMa-3 by using real-world SoC evidence from the COTA Vantage database to inform a more precise crossover adjustment model.
Methods:
Crossover adjustment was performed using real-world data to determine what post-progression survival (PPS) would have looked like in KarMMa-3 SoC patients had they not crossed over to ide-cel. First, PPS data from a TCE RRMM cohort in the COTA database (November 2015 to March 2021) were aligned with KarMMa-3 (April 2023 cutoff) based on key trial inclusion criteria. Next, COTA PPS data were combined with KarMMa-3 SoC PPS via dynamic borrowing (ie, incorporated in a way that allows more influence when the external data closely resemble the trial population and less when they differ) to estimate the impact of crossover while controlling for confounders. This estimated impact of crossover was then used to adjust OS times in KarMMa-3. Finally, a stratified Cox proportional hazards model was fitted to the adjusted KarMMa-3 OS times to estimate HRs comparing ide-cel versus SoC in KarMMa-3 patients. Separate analyses were performed for the KarMMa-3 intention-to-treat (ITT) population and modified-ITT (mITT) population (patients who received their initial assigned treatment).
Results:
Following crossover adjustment, ide-cel improved OS versus SoC (HR, 0.67; 95% CI, 0.49–0.93) for the KarMMa-3 ITT population (ide-cel, N = 254; SoC, N = 132). An OS benefit of ide-cel versus SoC was also observed in the mITT population after crossover adjustment (HR, 0.50; 95% CI, 0.35–0.70) (ide-cel, N = 225; SoC, N = 126). Crossover adjustment was based on data from KarMMa-3 patients, with PPS information borrowed from 471 COTA patients, and adjusted for age, number of prior lines of therapy, cytogenetic risk profile, triple-class refractory status, tumor burden, time to progression on last regimen, time since diagnosis, hemoglobin level, prior stem cell transplantation, race, sex, Eastern Cooperative Oncology Group score, and lactate dehydrogenase level.
Conclusions:
Leveraging real-world SoC data allowed for a more efficient and precise estimation of crossover-adjusted OS in KarMMa-3. Findings from this analysis further support the significant and clinically meaningful OS benefit of ide-cel over SoC in patients with RRMM.
