Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
IMPACT OF NEIGHBORHOOD-LEVEL DISADVANTAGE, TRAVEL DISTANCE, AND TRAVEL TIME ON CLINICAL OUTCOMES OF MULTIPLE MYELOMA (MM) PATIENTS TREATED WITH STANDARD OF CARE (SOC) IDECABTAGENE VICLEUCEL (IDE-CEL)
(PA-068) Impact of Neighborhood-level Disadvantage, Travel Distance, and Travel Time on Clinical Outcomes of Multiple Myeloma (MM) Patients Treated with Standard of Care (SOC) Idecabtagene Vicleucel (IDE-CEL)

Jessica Y. Islam, PhD, MPH (she/her/hers)
Assistant Professor
Moffitt Cancer Center
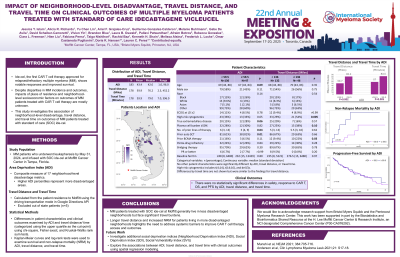
Ide-cel, the first CAR T cell therapy approved for MM, shows notable responses and improved survival. Despite racial, ethnic, and socioeconomic disparities in MM incidence and outcomes, impacts of place of residence and neighborhood-level socioeconomic factors on outcomes of MM patients (pts) treated with CAR T cell therapy are mostly unknown. Here we look at effects of neighborhood-level disadvantage and travel distance (TD)/time on outcomes of MM pts treated with SOC ide-cel.
Methods:
Pts with MM who underwent leukapheresis by May 31, 2024, and received ide-cel at Moffitt Cancer Center were included. The main exposure was Area Deprivation Index (ADI), a composite measure of 17 neighborhood-level disadvantage metrics. Higher ADI percentiles denote more disadvantaged areas. TD/time from pts’ homes to Moffitt were calculated using Google Directions API (driving mode). Differences in pt characteristics and clinical outcomes examined by ADI and TD/time were categorized using the upper quartile as the cut-point.
Results:
Of 183 MM pts treated with ide-cel, most were male (55%), non-Hispanic White (69%), and aged >60 y (75%). Safety and responses were aligned with previous data. Median follow-up was 12.4 mo (range 0.1–38.4). Median ADI was 42 (range 1–96) and 38% of pts lived in neighborhoods more disadvantaged than the national average (ADI >50). Baseline clinical characteristics showed that pts living in more disadvantaged neighborhoods (ADI ≥59.5, n=47) were younger (67 vs 69 y; P=0.09), had fewer prior therapies (5 vs 6; P=0.04), and were more likely to have had prior autologous stem cell transplant (81% vs 61%; P=0.01) and extramedullary disease (28% vs 15%; P=0.06) vs pts in less disadvantaged neighborhoods (ADI < 59.5, n=136). Post infusion, pts with high vs low ADI had higher peak C-reactive protein levels (11.3 vs 7.7 mg/dL; P=0.07). Clinical outcomes by ADI were similar, except non-relapse mortality (NRM), which was higher in pts living in more disadvantaged neighborhoods (13% vs 4%; P=0.06), mainly due to infections in both groups. Among in-state pts (n=178), median TD was 76.2 miles (range 2.3–452.2) and median travel time (TT) was 79 min (range 7–396). A total of 32% (n=52) of pts traveled >100 miles, and 28% traveled >2 h for CAR T cell therapy. Pts with a longer TD (≥136 miles) were more likely to have high-risk cytogenetics (54% vs 29%; P=0.005) and prior B-cell maturation antigen therapy (22% vs 9%; P=0.03); no other differences in pt characteristics/clinical outcomes by TD were noted. Findings were similar for TT. Pts from more disadvantaged neighborhoods had shorter TTs (54 vs 83 min; P=0.001) and TDs (46.2 vs 80.8 miles; P< 0.001).
Conclusions:
In these MM pts treated with SOC ide-cel, most lived in less disadvantaged neighborhoods yet faced significant travel burdens. Longer TD for most pts, and increased NRM in pts living in more disadvantaged neighborhoods highlights the need to address systemic barriers to improve CAR T cell therapy access and outcomes.
