Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
Serologic Immunity to Measles, Mumps, and Rubella in Multiple Myeloma Patients Following Cellular Therapy: A Descriptive Analysis
(PA-062) Serologic Immunity to Measles, Mumps, and Rubella in Multiple Myeloma Patients Following Cellular Therapy: A Descriptive Analysis

Patrick A. Hagen, MD; MPH
Associate Professor
Loyola University Chicago
Introduction:
Multiple myeloma is a malignant neoplasm of plasma cells that accounts for approximately 10% of all hematologic cancers. Patients with multiple myeloma (MM) are at heightened risk for infectious complications, particularly following intensive therapies such as autologous stem cell transplantation (ASCT) or chimeric antigen receptor (CAR) T-cell therapy. While immunity to measles, mumps, and rubella (MMR) may diminish post-treatment, real-world data on post-therapy serologic immunity remains limited. This study aims to characterize MMR immunity in multiple myeloma patients post-ASCT amid heightened risk from recent U.S. measles outbreaks.
Methods:
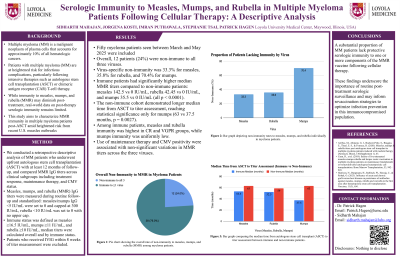
We conducted a retrospective descriptive analysis of multiple myeloma patients who underwent autologous stem cell transplantation (ASCT) as upfront consolidation, with at least 12 months post-ASCT. Measles, mumps, and rubella (MMR) IgG titers were measured during routine follow-up and standardized: measles and mumps IgG < 5 IU/mL were set to 0 and capped at 300 IU/mL; rubella < 10 IU/mL was set to 0 with no upper cap. Patients were classified as immune with titer thresholds of measles ≥16.5 IU/mL, mumps ≥11 IU/mL, and rubella ≥10 IU/mL. Median titers were calculated overall and by immune status. Patients receiving IVIG within 8 weeks of titer measurement were excluded. Comparisons were made across clinical subgroups, including response status, maintenance therapy, and CMV status.
Results:
50 patients seen in our myeloma clinic between March and May of 2025 were included. Overall, 12/50 (24% of patients) were non-immune to all three viruses. Individually, 33.3% lacked immunity to measles, 35.8% to rubella, and 70.4% to mumps. Immune patients had higher median MMR titers compared to non-immune for measles [142.5 (18.5–300) vs 0 (0–10.6) IU/mL, p < 0.0001], rubella [42.45 (10–509) vs 0 (0–0), p < 0.0001], and mumps [35.5 (12.7–283) vs 0 (0–10.4), p < 0.0001]. Non-immune cohort demonstrated longer median time from ASCT to titer assessment, with statistical significance only for mumps: measles (63 vs 53.5 months, p = 0.4135), rubella (59 vs 52.5, p = 0.5512), and mumps (63 vs 37.5, p = 0.0027). Among immune patients, immunity to measles (62.5% CR, 58.8% VGPR 40% PR) and rubella (58.8% VGPR, 56.25% CR, 50% PR) was highest in VGPR and CR groups, while mumps immunity was uniformly low (37.5% CR, 26.5% VGPR, 10% PR). Use of maintenance therapy was associated with non-significant higher measles and rubella titers, and no difference in mumps while CMV positivity correlated with non-significant higher titers for measles, mumps, and lower for rubella.
Conclusions:
A substantial proportion of MM patients lack protective serologic immunity to one or more components of the MMR vaccine following cellular therapy. These findings underscore the importance of routine post-treatment serologic surveillance and may inform revaccination strategies to optimize infection prevention in this immunocompromised population.
