Myeloma Novel Drug Targets and agents
Category: Myeloma Novel Drug Targets and agents
Comparative Analysis of Motixafortide versus Plerixafor for Stem Cell Mobilization and Collection in Multiple Myeloma: A Single Center Real-World Experience
(PA-291) Comparative Analysis of Motixafortide versus Plerixafor for Stem Cell Mobilization and Collection in Multiple Myeloma: A Single Center Real-world Experience

Sara Close, MS, PA-C (she/her/hers)
Physician Assistant
Dana Farber Cancer Institute
Stem cell collection after 4–8 cycles of induction therapy remains the standard for multiple myeloma (MM) patients prior to autologous stem cell transplant (ASCT). Increasing demand for apheresis services, especially with the rise of CAR-T and other cell therapies, highlights the need for efficient mobilization strategies. Motixafortide, a CXCR4 antagonist with prolonged receptor occupancy (≥72 hours vs. plerixafor’s ~6–12 hours), may enhance stem cell mobilization kinetics.
Methods:
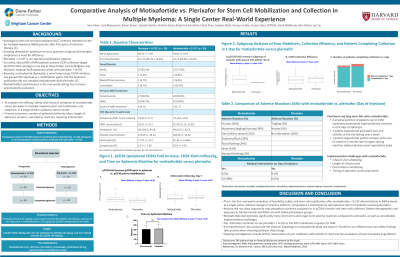
This quality initiative compared a prospective cohort of 30 MM patients mobilized with motixafortide + G-CSF to 30 retrospective MM patients mobilized with plerixafor + G-CSF. The goal was to evaluate feasibility, mobilization efficacy, and safety of motixafortide in a real-world single-center setting. Cohorts were matched by age, gender, race, and prior exposure to daratumumab and IMiDs (lenalidomide/pomalidomide). Plerixafor (0.16–0.24 mg/kg SC) was administered if peripheral CD34 (pCD34) count was < 30 cells/µL on the evening before collection (Day 4 of 5 of G-CSF). Motixafortide (1.25 mg/kg SC) was given regardless of pCD34, based on clinical logistics. Premedication for motixafortide included cetirizine, famotidine, montelukast, acetaminophen, prednisone, and lidocaine cream with ice during a 1-hour monitoring period. Target collection was ≥4.0×10^6 CD34+ cells/kg, with minimum 12L processed for pCD34 >50 cells/µL and 4 total blood volumes for pCD34 < 50 cells/µL.
Results:
Twenty-nine of 30 motixafortide patients completed mobilization. Fold-increase in pCD34 was similar between groups, though three “super-responders” were noted in the motixafortide cohort. A trend toward superior pCD34 increase with motixafortide was observed in patients with very low Day 4 pCD34 (< 5 cells/µL), but sample size limited conclusions. CD34 cell yield and collection efficiency did not differ significantly. Twenty-seven patients in each group completed collection in a single day. Time on apheresis, blood volume processed, and CD34 product percentages were comparable. Adverse events requiring intervention occurred in 48% of motixafortide recipients, primarily pruritus (45%), tingling/burning (34%), pain (31%), erythema/rash (24%), and facial flushing (24%). No interventions were needed after plerixafor. One motixafortide patient experienced painful injection-site nodules lasting up to 3 months.
Conclusions:
In this real-world evaluation, motixafortide did not demonstrate superiority over plerixafor in pCD34 mobilization, stem cell yield, or collection efficiency in MM patients. Higher rates of adverse reactions with motixafortide influenced continued institutional preference for plerixafor in initial ASCT mobilization. Further studies will focus on motixafortide’s role in poor mobilizers and post-transplant engraftment.
