Myeloma Novel Drug Targets and agents
Category: Myeloma Novel Drug Targets and agents
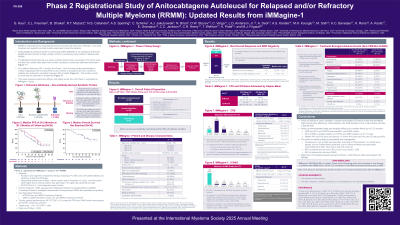
Phase 2 Registrational Study of Anitocabtagene Autoleucel for Relapsed and/or Refractory Multiple Myeloma (RRMM): Updated Results from iMMagine-1
(PA-288) Phase 2 Registrational Study of Anitocabtagene Autoleucel for Relapsed and/or Refractory Multiple Myeloma (RRMM): Updated Results from iMMagine-1
Gurbakhash Kaur, MD
Assistant Professor
Icahn School of Medicine at Mount Sinai
Anitocabtagene autoleucel (anito-cel) is an autologous anti–BCMA chimeric antigen receptor (CAR) T-cell therapy with a novel D-domain binder under development for patients (pts) with RRMM. Updated results from the ongoing iMMagine-1 registrational trial are presented.
Methods:
Details of iMMagine-1 (NCT05396885) have been previously reported (Freeman et al., ASH 2024). Eligible pts were triple-class exposed, had progressed after ≥3 LoT, and were refractory to last LoT. Following leukapheresis, optional bridging, and anito-cel manufacturing, pts received lymphodepletion chemotherapy and a single infusion of anito-cel. The primary endpoint is overall response rate (ORR) by Independent Review Committee and assessed using 2016 IMWG criteria. MRD is assessed by next-generation sequencing, toxicity is graded per CTCAE version 5.0, and CRS and ICANS are graded by the ASTCT consensus criteria. This analysis reports investigator-assessed safety and efficacy outcomes.
Results:
As of October 31, 2024, 86 pts received anito-cel under the final manufacturing process with ≥2 months of follow-up and comprised the efficacy evaluable population; median follow-up was 9.5 months (range, 2-23). Pts had received a median of 4 prior LoT (range, 3-8) with 37 pts (43%) having received only 3 prior LoT. Seventy-four pts (86%) were triple-class refractory and 37 (43%) were penta-drug refractory. Investigator-assessed ORR was 97% (83/86) with a CR/sCR rate of 62% (53/86). Of those evaluable for MRD testing (n=58), 54 (93.1%) achieved MRD negativity at least to the level of 10-5 and median time to MRD negativity was 1 month (range, 1 to 6 months). Using Kaplan-Meier methods, the duration of response (DoR), PFS, and OS rates at 12-month milestone timepoints are 75.6%, 78.5%, and 96.5%, respectively. Median DOR, PFS and OS have not been reached.
The safety evaluable population (N=98) had ≥1 month of follow-up by the data cut-off. The most common grade ≥3 treatment emergent adverse events (AEs) were cytopenias. Eighty-four pts (86%) had CRS Gr1 or less, including 17 (17%) with no CRS, and 96 (98%) had either no CRS or CRS resolution ≤14 days of anito-cel infusion. Any grade CRS was observed in 81 pts (83%) with 67 (68%) Gr1, 13 (13%) Gr2, and 1 (1%) Gr5. Median onset was 4 days (range, 1-17) with a median duration of 3 days (range, 1-9). Any grade ICANS was observed in 9 pts (9%) with 4 (4%) Gr1, 4 (4%) Gr2, and 1 (1%) Gr3. No delayed or non-ICANS neurotoxicities including no Parkinsonism, no cranial nerve palsies, and no Guillain-Barré syndrome have been observed.
Conclusions:
Ongoing results from iMMagine-1 demonstrate deep and durable efficacy and manageable safety in a 4L+ RRMM population. No delayed or non-ICANS neurotoxicities including no Parkinsonism, no cranial nerve palsies, and no Guillain-Barré syndrome have been observed across the Phase 1 or Phase 2 iMMagine-1 studies to date. Data including efficacy and safety in all treated pts will be presented.
