Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
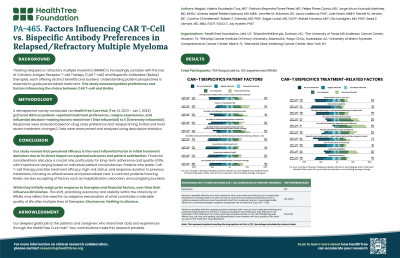
Factors Influencing CAR T-Cell vs. Bispecific Antibody Preferences in Relapsed/Refractory Multiple Myeloma
(PA-465) Factors Influencing CAR T-Cell vs. Bispecific Antibody Preferences in Relapsed/Refractory Multiple Myeloma

Magaly Valeria Escobedo Cruz, MD (she/her/hers)
Clinical Data Manager
HealthTree Foundation
Treating relapsed or refractory multiple myeloma (RRMM) is increasingly complex with the rise of Chimeric Antigen Receptor T-cell Therapy (CAR T-cell) and Bispecific Antibodies (BsAbs) therapies, each offering distinct benefits and burdens. Understanding patient perspectives is essential to guide personalized treatment. This study assessed patient preferences and factors influencing the choice between CAR T-cell and BsAbs.
Methods:
A retrospective survey conducted via HealthTree Cure Hub registry (Feb 14, 2023 - Jan 1, 2024) gathered data on patient-reported treatment preferences, relapse experiences, and influential decision-making factors rated from 1 (Not influential) to 5 (Extremely influential). Responses were analyzed based on drug class preference and relapse timing (initial and most recent treatment changes). Data were anonymized and analyzed using descriptive statistics.
Results:
Of 784 respondents, 333 experienced relapse (RRMM), and 201 indicated a drug class preference. CAR T-cell therapy was preferred by 66% (n=132), while BsAbs were favored by 34% (n=69). Patients favoring CAR T-cell rated higher influence for treatment efficacy (4.6±0.7 vs. 4.2±1.1, p< 0.05), genetic-based high-risk status (2.0±1.7 vs. 1.3±1.5, p< 0.05), and prior treatment response duration (2.7±1.2 vs. 2.1±1.5, p< 0.05). Additionally, the importance of care team explanations increased over time for this group (initial: 4.0±1.2; recent: 4.3±0.9, p< 0.05).
In contrast, patients favoring bispecifics were less accepting of side effects requiring hospitalization (4.2±1.7 v. 5.0±1.8, p< 0.05), higher family care burden (3.1±1.7 v. 3.7±1.6, p < 0.05), or a one-time therapy involving relocation costs for several weeks (4.4±1.7 v. 5.5±1.6, p< 0.05). Furthermore, these patients rated out-of-pocket costs and economic status as less influential over time (initial: 2.5±1.4; recent: 2.0±1.4, p< 0.05), and similarly, decreased the influence rating of previous response duration (initial: 2.6±1.4; recent: 2.1±1.5, p< 0.05).
Conclusions:
Our study reveals that perceived efficacy is the most influential factor in initial treatment decisions due to its direct impact on expected outcomes and patient satisfaction. Financial considerations also play a crucial role, particularly for long-term adherence and quality of life, with importance varying based on individual patient circumstances. Patients who prefer CAR T-cell therapy prioritize treatment efficacy, high-risk status, and response duration to previous treatments, focusing on effectiveness and personalized care. In contrast, patients favoring BsAbs are less accepting of factors such as hospitalization, relocation, and caregiving burdens.
While they initially weigh prior response to therapies and financial factors, over time their influence diminishes. This shift, prioritizing autonomy and stability within the chronicity of RRMM, may reflect the need for an adaptive reevaluation of what constitutes a tolerable quality of life after multiple lines of therapies.
