Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
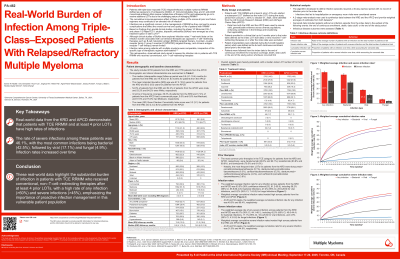
Real-world (RW) Burden of Infection Among Triple-class–exposed (TCE) Patients (Pts) With Relapsed/Refractory Multiple Myeloma (RRMM)
(PA-462) Real-world (RW) Burden of Infection Among Triple-class–exposed (TCE) Patients (Pts) With Relapsed/Refractory Multiple Myeloma (RRMM)

Samer Al Hadidi, MD MS
Associate Professor of Medicine
UT Southwestern Medical Center
Methods:
Pts with TCE RRMM and with ≥4 prior LOTs who had started a subsequent LOT (index LOT) during the study period (Jan 1, 2016-Oct 31, 2024) were identified from the Komodo Research Dataset (KMD) and the All-Payer Claims Data (APCD). Pts enrolled in a trial ≤6 mo prior to index (index LOT start date) or receiving T-cell–redirecting therapies on/post index were excluded. Pt characteristics were collected during the 6-mo baseline period. Pts were followed from the index date to end of continuous enrollment, death, data cut-off, or end of study period. An algorithm requiring a 30-day washout with no infections prior to index was developed to define infection episodes. Infections that led to hospitalization or emergency room visits were considered severe. Meta-analysis was used to synthesize data between KMD and APCD.
Results:
2702 KMD and 1755 APCD pts were included (median follow-up, 9.5 and 14.9 mo, respectively). Mean (SD) age was 67.2 (10.6) y for KMD and 69.3 (9.5) y for APCD. Of KMD/APCD pts, 54.0%/52.4% were male and 53.2%/64.2% were White; 29.3%/17.4% had a commercial payer, 9.0%/6.6% had Medicaid, and 61.5%/75.0% had Medicare. Mean (SD) Quan-Charlson Comorbidity Index was 3.2 (3.1)/2.3 (2.8). Pts were heavily pre-treated, with a median index LOT number of 5 in both databases. The most common prior therapies in the TCE classes for KMD/APCD pts were daratumumab (D; 99.3%/99.1%), lenalidomide (83.8%/89.9%), and bortezomib (79.5%/81.6%). The most frequent index LOTs in KMD pts were elotuzumab+pomalidomide (P)±dexamethasone (d; 5.1%), DP±d (6.3%), carfilzomib (K)±d (5.2%), DK±d (4.4%), and KP±d (3.9%). Across KMD and APCD pts, the weighted average (wavg) infection rate for any infection was 63.5% (58.2%, bacterial; 27.4%, viral; 8.2%, fungal); at 26 and 52 wks, the wavg cumulative infection rates for any infection were 49.5% and 66.4%, respectively. The wavg rate of severe infection was 46.1% for any infection (42.5%, bacterial; 17.1%, viral; 4.9%, fungal); at 26 and 52 wks, these wavg cumulative rates for severe infection were 31.5% and 44.9%, respectively.
Conclusions: These RW data highlight the substantial burden of infection in TCE pts with RRMM receiving conventional (non-T-cell–redirecting) therapies after ³4 prior LOTs, with a high risk of any infection ( >60%) and severe infection ( >45%).
