Myeloma Genomics and Microenvironment and immune profiling
Category: Myeloma Genomics and Microenvironment and immune profiling
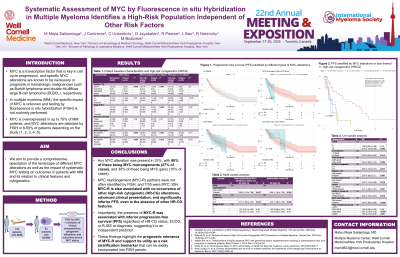
Systematic Assessment of MYC by Fluorescence in situ Hybridization in Multiple Myeloma Identifies a High-Risk Population Independent of Other Risk Factors
(PA-250) Systematic Assessment of MYC by Fluorescence in situ Hybridization in Multiple Myeloma Identifies a High-Risk Population Independent of Other Risk Factors
.jpg)
Mateo Mejia Saldarriaga, MD
Assisstant Professor
Weill Cornell Medicine
MYC testing is not routinely performed in multiple myeloma (MM) despite being recognized as a prognostic biomarker. We present the impact of systematic MYC testing for alterations on outcomes in patients (pts) with MM and its relation to clinical features and cytogenetics.
Methods: A total 133 pts who underwent bone marrow biopsy and had a diagnosis of MM (147 total samples) were systematically assessed for MYC alterations using fluorescence in situ hybridization (FISH) testing over a 24-month period. 126 were assessable for progression-free survival (PFS), and 92 were newly diagnosed with MM (NDMM). MYC alterations were classified as rearrangements (MYC-R) or gains. Clinical characteristics, cytogenetic alterations, and outcomes were compared across MYC status. PFS was defined as time from diagnosis to death or progression/relapse of disease as defined by the International Myeloma Working Group criteria.
Results:
MYC alterations were present in 44 of 133 MM pts (33%). MYC-R was present in 35 pts (26%), while MYC gain was present in 13 pts (9.8%). Most MYC-R partners were not identified on standard of care FISH, with MYC::IGH being present in 7/35 cases.
Compared to non-altered MYC (MYC-negative) cases, those with MYC-R were older (median 75 vs. 67 years, p = 0.005), and more likely to present with international staging system III (56% vs. 29%, p = 0.008) and hypoalbuminemia (68% vs. 42%, p = 0.01). MYC-R cases had higher rates of del(17p): 23% vs. 6.7% (p = 0.02), t(4;14): 23% vs. 9% (p = 0.07), and lower rates of t(11;14): 17% vs 37%, p = 0.03). MYC-R was associated with higher rates of high-risk cytogenetics (HR-CG - del(17p), t(4:14), t(14;16)); 46% vs 19%, p = 0.003), HR-CG plus gain(1q) (74% vs 55%, p = 0.04), and HR-CG plus gain(1q) or del(1p), 80% vs 56%, p = 0.01).
Pts with MYC-R had significantly shorter PFS compared to MYC-negative (15.6 vs. 35.7 months, p = 0.017). Other variables associated with PFS included ISS, R-ISS, LDH, albumin, del(17p), and HR-CG. In multivariable model, only MYC-R was associated with inferior PFS (HR 2.82, 95% CI 1.12-7.06, p = 0.027). Additionally, when patients were stratified by MYC-R and HR-CG status, patients with MYC-R and no HR-CG had inferior PFS compared to MYC-negative/no HR-CG patients (p = 0.001) and similar to when there was the presence of HR-CG.
Conclusions:
