MRD and Biomarkers
Category: MRD and Biomarkers
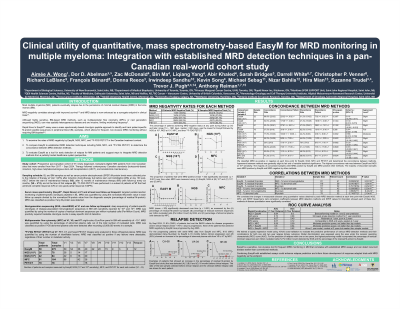
Clinical utility of quantitative, mass spectrometry-based EasyM for MRD monitoring in multiple myeloma: Integration with established MRD detection techniques in a pan-Canadian real-world cohort study
(PA-196) Clinical Utility of Quantitative, Mass Spectrometry-based EasyM for MRD Monitoring in Multiple Myeloma: Integration with Established MRD Detection Techniques in a Pan-canadian Real-world Cohort Study

Aimée A. Wong, PhD (she/her/hers)
Research Scientist
University of New Brunswick
Introduction:
Minimal residual disease (MRD) in the bone marrow (BM) following multiple myeloma (MM) treatment is an adverse prognostic factor and an emerging clinical trials endpoint. Blood-based MRD assays could reduce invasive BM testing and overcome spatial heterogeneity in the BM and BM hemodilution. The EasyM assay uses a mass spectrometry-based approach to identify and track patient-specific, clonotypic M-protein peptides in peripheral blood (PB), facilitating frequent, non-invasive MRD monitoring. The optimal integration of different MRD tests remains unclear.
Methods:
We evaluated MRD in a pan-Canadian cohort of 91 newly diagnosed, transplant-eligible MM patients using EasyM (N=59 patients), next-generation sequencing (NGS) of immunoglobulin clonotypes from BM (10⁻⁵ and 10⁻⁶ sensitivity, N=42 patients), multiparameter flow cytometry of BM (MFC, sensitivity between 10⁻4 and 10⁻⁶, N=48 patients), and 18F-FDG PET/CT (PET, N=18 patients) (sample collection from Nov 2017–Sept 2024). Samples were analyzed prior to the initiation of therapy and at one or more follow up timepoints: after induction chemotherapy, 100 days post-ASCT, after 12 months of maintenance therapy, and every 6 months until progression. PET was done after 12 months of maintenance therapy if in VGPR or better. We compared EasyM with NGS, MFC and PET and assessed their prediction of subsequent relapse.
Results:
Over the follow-up period (range 114 – 1961 days, median = 920 days), MRD negative status was achieved by 18% (11/59) of patients by EasyM, 21% (9/42) by NGS at 10⁻⁶, 57% (24/42) by NGS at 10⁻⁵, 58% (28/48) by MFC, and 83% (15/18) by PET. Among matched EasyM and BM samples, concordance was highest between EasyM and NGS at 10⁻⁶ (70%, N=30 matched samples), followed by MFC (58%, N=60), NGS at 10⁻5 (53%, N=38), and then PET (37%, N=16). The majority of discordant samples were positive by EasyM and negative by other methods (range of 23% with NGS at 10-6 – 63% with PET). The percentage of residual M-protein by EasyM was strongly correlated with the percentage of clonal plasma cells from MFC, MRD quantitation via NGS, and serum protein electrophoresis (SPEP) results (Spearman r ≥ 0.8, p < 0.01). None of the patients that achieved MRD negativity by EasyM have progressed to date. By Sept 2024, 20 patients progressed and for the 13 progressing patients with serial data, 9 demonstrated rising M-protein by EasyM 2 – 12 months before clinical progression. A two‑variable logistic model combining percent residual M‑protein via EasyM with NGS MRD quantitation at 10-6 yielded the best relapse prediction (AUC = 0.84 within 1 year of sample collection; 0.80 within 2 years).
Conclusions:
EasyM is a sensitive, non-invasive tool for frequent MRD monitoring in MM that correlates with established MRD assays and can detect recurrent disease earlier than conventional methods. Combining EasyM with established assays could enhance relapse prediction and inform future development of response adapted trials with MRD negativity as the endpoint.
