Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
DARATUMUMAB, LENALIDOMIDE, BORTEZOMIB, AND DEXAMETHASONE FOR NEWLY DIAGNOSED MULTIPLE MYELOMA: OUTCOME AND SAFETY PROFILE FROM A MULTI-CENTER REAL-WORLD EXPERIENCE
(PA-454) Daratumumab, Lenalidomide, Bortezomib, and Dexamethasone for Newly Diagnosed Multiple Myeloma: Outcome and Safety Profile from a Multi-center Real-world Experience

Yue Wu, M.Med
Doctor
Fu Xing Hospital, Capital Medical University, Beijing, China
Introduction:
The lenalidomide,bortezomib and dexamethasone (RVD) regimen was once the first-line treatment for multiple myeloma, and achieved favorable outcomes. The addition of daratumumab to the RVD regimen (D-VRD) has been shown to improve response rates and depth of response. Currently, the D-VRD regimen has been recommended by the NCCN as a first-line treatment for newly diagnosed multiple myeloma (NDMM).
Methods:
A retrospective study was conducted with medical review of all patients diagnosed with multiple myeloma and treated with D-VRD at Peking University People's Hospital,Sheng Jing Hospital of China Medical University and Fu Xing Hospital, Capital Medical University,from June 2021 to February 2025,response rate and safety profile were evaluated. The results were compared with the outcomes of NDMM patients treated with the RVD regimen in the Peking University People's Hospital from August 2016 to September 2020.
Results:
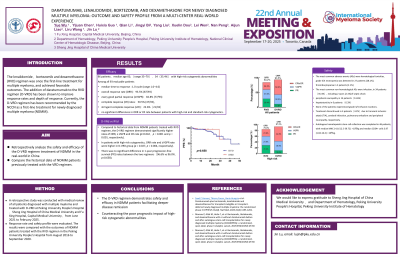
A total of 96 patients were enrolled (median age 60, range 35–70 years), , including 34 with high-risk cytogenetic abnormalities. Among all 93 evaluable patients, the overall response rate (ORR), ≥very good partial response (≥VGPR), and complete response (CR) rates were 93.5% (87/93), 82.8% (77/93), and 50.5% (47/93), respectively, including 21 cases of stringent complete response (sCR).
The median time to response was 1.0 cycle (range 1.0–4.0). There were no significant differences in ORR or CR rate between patients with high-risk and standard-risk cytogenetics. Compared to historical data from NDMM patients treated with RVD regimen, the D-VRD regimen demonstrated significantly higher rates of ORR, ≥ VGPR and CR rate (p=0.042,p<0.001 and p<0.001, respectively). In patients with high-risk cytogenetics, ORR rate and ≥VGPR rate were higher in D-VRD group (p = 0.027, p = 0.004, respectively). There was no significant difference in 1-year progression-free survival (PFS) rates between the two regimens(96.6% vs 96.0%,p=0.658). Autologous hematopoietic stem cell collection was completed in 46 patients, with median MNC 14.16 (2.5-39.72) ×10⁸/kg and median CD34+ cells 3.97 (1.04-16.4) ×10⁶/kg. The most common adverse events (AEs) were hematological toxicities,grade 3/4 neutropenia was detected in 27 patients (28.1%),thrombocytopenia in 2 patients (2.1%). The most common non-hematological AEs were infection, in 34 patients, including 2 cases of septic shock,peripheral neuropathy in 14 patients, hepatotoxicity in 6 patients. None of the patients experienced grade 3/4 infusion reactions. Treatment discontinued in 4 patients due to transient ischemic attack (TIA), cerebral infarction, pulmonary embolism and peripheral neuropathy, respectively.
Table 1 Efficacy of RVD and D-VRD Regimen
| RVD | D-VRD | P value |
ORR (%) | 84.2 | 97.0 | 0.027 |
≥VGPR (%) | 55.8 | 78.8 | 0.004 |
≥CR(%) | 24.2 | 42.4 | 0.077 |
Conclusions:
The D-VRD regimen demonstrates safety and efficacy in NDMM patients, facilitating deeper disease remission and counteracting the poor prognostic impact of high-risk cytogenetic abnormalities.
