Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
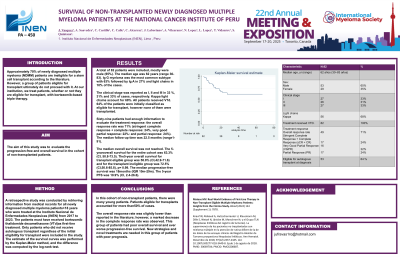
Survival of Non-transplanted Newly Diagnosed Multiple Myeloma Patients at the National Cancer Institute of Peru
(PA-450) Survival of Non-transplanted Newly Diagnosed Multiple Myeloma Patients at the National Cancer Institute of Peru

Jule Vasquez, MD (he/him/his)
Oncologist
AUNA
Introduction:
Approximately 70% of newly diagnosed multiple myeloma (NDMM) patients are ineligible for a stem cell transplant according to the literature. However, a group of patients eligible for transplant ultimately do not proceed with it. At our institution, we treat patients, whether or not they are eligible for transplant, with bortezomib-based triple therapy. The aim of this study was to evaluate the progression-free and overall survival in the cohort of non-transplanted patients.
Methods:
A retrospective study was conducted by retrieving information from medical records for all newly diagnosed multiple myeloma patients >18 years who were treated at the Instituto Nacional de Enfermedades Neoplasicas (INEN) from 2017 to 2023. The patients must have received bortezomib thalidomide dexamethasone (VTd) as first-line treatment. Only patients who did not receive autologous transplant regardless of the initial eligibility for transplant were included in the study. The estimate of the survival curves was performed by the Kaplan-Meier method, and the difference was computed by the log-rank test.
Results:
A total of 82 patients were included, mostly were male (65%). The median age was 62 years (range 30-83). Ig G myeloma was the most common subtype with 63% followed by Ig A in 27% and and light chains in 10% of the cases. The clinical stage was reported as I, II and III in 33 %, 31% and 33% of cases, respectively. Kappa light chains account for 68%. All patients received VTd. 64% of the patients were initially classified as eligible for transplant, however none of them were transplanted. Sixty-nine patients had enough information to evaluate the treatment response: the overall response rate was 71% (stringent complete response + complete response: 24%, very good partial response: 22%: and partial response: 24%). The median follow-up time was 22.5 months (range 1-91). The median overall survival was not reached. The 5-year overall survival for the entire cohort was 63.3% (CI, 50.8-73.5). The 5-year overall survival for transplant eligible group was 58.8% (CI, 42.9-71.6) and for the transplant ineligible group was 72.5% (CI, 50.6-85.8), p= 0.99. The median progression-free survival was 18 months (IQR 10m-29m). The 5-year PFS was 10.9% (CI, 2.4-26.6).
Conclusions: In this cohort of non-transplant patients, there were many young patients. Patients eligible for transplants accounted for more than 50% of cases.
The overall response rate was slightly lower than reported in the literature; however, a marked decrease in the complete response rate was observed. This group of patients had poor overall survival and ever worse progression-free survival. New strategies and novel treatments are needed in this group of patients with poor prognosis.
