Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
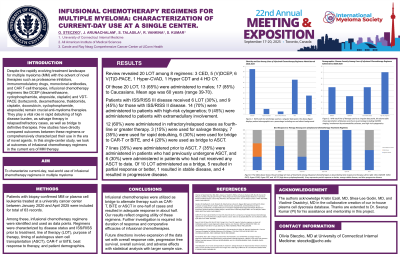
Infusional chemotherapy regimens for multiple myeloma: characterization of current-day use at a single center.
(PA-440) Infusional Chemotherapy Regimens for Multiple Myeloma: Characterization of Current-day Use at a Single Center

Olivia Steczko, MD
Resident Physician, PGY-3
UConn Health
Introduction:
Despite the rapidly evolving treatment landscape for multiple myeloma (MM) with the advent of novel therapies such as proteasome inhibitors, immunomodulatory drugs, monoclonal antibodies, and CAR T-cell therapies, infusional chemotherapy regimens like DCEP (dexamethasone, cyclophosphamide, etoposide, cisplatin) and VDT-PACE (bortezomib, dexamethasone, thalidomide, cisplatin, doxorubicin, cyclophosphamide, etoposide) remain crucial anti-myeloma therapies. They play a vital role in rapid debulking of high disease burden, as salvage therapy in relapsed/refractory cases, as well as bridge to definitive therapies. Few studies have directly compared outcomes between these regimens or comprehensively characterized their use in the era of novel agents. In this single-center study, we look at outcomes of infusional chemotherapy regimens in the current era of MM therapy.
Methods:
Patients with biopsy-confirmed MM or plasma cell leukemia treated at a university cancer center between January 2020 and April 2025 were included for total of 63 records. Among these, infusional chemotherapy regimens were identified and used as data points. Regimens were characterized by disease status and ISS/RISS prior to treatment, line of therapy (LOT), purpose of therapy, timing of autologous stem cell transplantation (ASCT), CAR-T or BiTE, best response to therapy, and patient demographics.
Results: Review revealed 20 LOT among 8 regimens: 3 CED, 5 (V)DCEP, 6 V(T)D-PACE, 1 Hyper-CVAD, 1 Hyper CDT and 4 HD CY. Of these 20 LOT, 13 (65%) were administered to males; 17 (85%) to Caucasians. Mean age was 60 years (range 39-70). Patients with ISS/RISS III disease received 6 LOT (30%), and 9 (45%) for those with ISS/RISS II disease. 14 (70%) were administered to patients with high-risk cytogenetics; 9 (45%) were administered to patients with extramedullary involvement. 12 (60%) were administered in refractory/relapsed cases as fourth-line or greater therapy. 3 (15%) were used for salvage therapy, 7 (35%) were used for rapid debulking, 6 (30%) were used for bridge to CAR-T or BiTE, and 4 (20%) were used as bridge to ASCT. 7 lines (35%) were administered prior to ASCT, 7 (35%) were administered in patients who had previously undergone ASCT, and 6 (30%) were administered in patients who had not received any ASCT to date. Of 10 LOT administered as a bridge, 5 resulted in partial response or better, 1 resulted in stable disease, and 4 resulted in progressive disease.
Conclusions:
Infusional chemotherapies were utilized as bridge to alternate therapy such as CAR-T, BiTE or ASCT in one-half of cases and resulted in adequate response in about half. Our results reflect ongoing utility of these regimens. Further investigation is required into duration of response and comparative efficacies of infusional chemotherapies. Future directions will involve expansion of the data set with overall response rate, progression free survival, overall survival, and adverse effects with statistical analysis with larger sample size.
