Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
HIV and Multiple Myeloma: Do Patients Present at a Younger Age? A Perspective From a South African Orthopaedic Oncology Unit.
(PA-423) HIV and Multiple Myeloma: Do Patients Present at a Younger Age? A Perspective From a South African Orthopaedic Oncology Unit.

Oatile Phakathi, MBChB (UCT) FC Orth (SA) MMed (Wits)
Musculoskeletal Oncology Fellow
University of Toronto
Introduction:
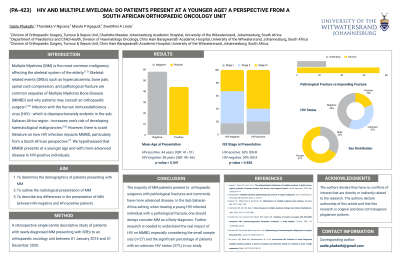
Multiple Myeloma (MM) is the third most common haematological malignancy and the most common malignancy affecting the skeletal systems of the elderly. Skeletal-related events (SREs) such as hypercalcaemia, bone pain, spinal cord compression, and pathological fracture are common sequelae of Multiple Myeloma Bone Disease (MMBD) and are the reasons patients may consult an orthopaedic surgeon. It has been established that infection with the human immunodeficiency virus (HIV) increases one’s risk of developing haematological malignancies. However, there is scant literature on how HIV infection affects MMBD, particularly from a South African perspective. We hypothesised that MMBD presents at a younger age and with more advanced disease in HIV-positive individuals.
Methods:
A retrospective single-centre descriptive study of patients with newly-diagnosed MM presenting with SREs to an orthopaedic oncology unit between 01 January 2016 and 31 December 2020. Patient demographic data (e.g., age, race and sex), biochemical and histopathological results, and whole-body X-rays (WBXR) were collected for each participant.
Results:
Twenty-seven patients were included. The median age at presentation was 56 years (inter-quartile range, IQR: 49 ‒ 47). Regarding HIV infection, 19% (n = 5) were HIV-positive, 45% (n = 12) were HIV-negative, and 37% (n = 10) had an unknown status due to absent screening. The age at presentation in HIV-positive patients was 44 years (IQR: 41 - 51); in HIV-negative patients, it was 58 years (IQR: 48 – 66). The difference in age at presentation between HIV-positive and HIV-negative patients was statistically significant, with a Kruskal-Wallis p-value of 0.041. Among HIV-positive patients, 60% (n = 3) presented with ISS stage III disease, while 50% (n = 10) of HIV-negative patients presented with ISS stage II disease, Fisher’s exact p-value = 0.836; an insignificant difference. The presenting complaint was mainly a pathological fracture at 67% (n = 20), predominantly affecting the femur in 50% (n = 10).
Conclusions:
The majority of MM patients present to the orthopaedic surgeon with pathological fractures and commonly have more advanced disease. In the Sub-Saharan Africa setting, when treating a young HIV-infected individual with a pathological fracture, one should always consider MM as a likely diagnosis. Further research is needed to understand the real impact of HIV on MM, especially considering the small sample size (n=27) and the significant percentage of patients with an unknown HIV status (37%) in our study.
