Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Real-World (RW) Outcomes of Newly Diagnosed Multiple Myeloma (NDMM) Patients (pts) Treated with Front-Line Daratumumab (dara) Lenalidomide (len) and Dexamethasone (dex) (DRd)
(PA-420) Real-World (RW) Outcomes of Newly Diagnosed Multiple Myeloma (NDMM) Patients (pts) Treated with Front-Line Daratumumab (dara) Lenalidomide (len) and Dexamethasone (dex) (DRd)

Ricardo D. Parrondo, MD
Assistant Professor of Medicine
Mayo Clinic Florida
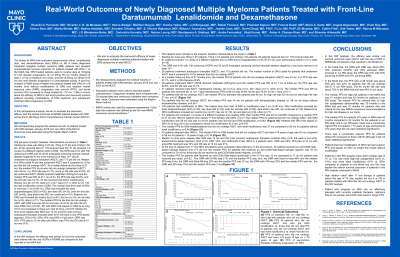
The phase III MAIA trial evaluated DRd vs. Rd in NDMM pts that were transplant ineligible (TI). Little is known about the efficacy of DRd in RW practice including modifications of DRd treatment and subsequent treatment after progression on DRd. We aim to evaluate the RW efficacy of NDMM pts treated with DRd across the tri-site Mayo Clinic Comprehensive Cancer (MCCC).
Methods:
We retrospectively analyzed the medical records of pts treated with DRd between January 2016 and July 2023 at the MCCC. Outcomes were estimated using the Kaplan-Meier method.
Results:
202 pts were included; 128 pts were male, and the median age of MM diagnosis was 75.42 pts had ISS III, 37 pts had R-ISS III, 87 pts had high risk FISH, 20 pts had extramedullary disease, 33 pts had ultra high-risk disease, 18 pts had renal insufficiency (RI) with creatinine >2 mg/dL.Starting len dose was 25mg in 97 pts, 15mg in 51 pts and ≤10mg in 52 pts. 20 pts received dara IV, 179 received dara SQ. 51 pts received 1-2 cycles of a different regimen prior to DRd due to hospitalization (n=5), RI (n=12), poor performance status (n=17), other (n=18).The ORR was 91% with 130 achieving ≥VGPR and 32 (of 63 evaluable) achieving minimal residual disease negativity in the bone marrow to at least 10-5. 129 pts were considered TI and 72 pts were considered transplant eligible (TE). At a median follow-up (f/u) time of 27 mo, the median PFS of pts who did not undergo transplant (ASCT) was 43 mo, 4 yr PFS rate was 41.7%, and 4 yr OS rate was 43.9%. 28 TE pts underwent ASCT (26/28 received melphalan 200mg/m2) and the median PFS was NR; at 47.1 mo of f/u, the PFS rate was 64.6%. 27 pts received post-ASCT maintenance therapy (tx); len (n=12), dara (n=1), len+ dara (n=11), other (n=3). 135 pts had modification (mod) of DRd. The median time from start of DRd to mod was 6 mo. DRd mod included len dose stopped/dropped (S/D) (n=35), dex dose S/D (n=23), both len and dex S/D (n=62), dara and/or dex S/D, len continued (n=19). Reasons for DRd mod included len toxicity (tox) (n=47), dex tox (n=10), len and dex tox (n=9), other (n=71). The median PFS for TI pts with DRd mod was 48 mo and was 14 mo for pts who did not have DRd mod, p< 0.001. Pts with DRd mod stayed on DRd 3x as long (15.7 mo) compared to those w/o mod (5.7mo).The median PFS for TI DRd treated pts with RI was 37 mo compared to 43 mo for pts without RI, p=0.70. 45 pts relapsed after DRd tx. Median f/u time since relapse after DRd was 13 mo and the most common subsequent therapies included bortezomib (V)-DRd (n=5), Dara-Vd, DRd, V-pomalidomide (P)-dex, and carfilzomib-P-dex in 4 pts each.PFS rate at 12 mo with post-DRd tx was 74%.
Conclusions: In this RW analysis, the efficacy and survival outcomes of TI NDMM pts treated with DRd was comparable to that reported in the MAIA trial.
