Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
Clinicopathological analysis of Parkinsonism-like neurotoxicity after BCMA-directed CAR-T therapy: an Autopsy Case With idecabtagene-vicleucel
(PA-092) Clinicopathological Analysis of Parkinsonism-like Neurotoxicity after BCMA-Directed CAR-T Therapy: An Autopsy Case With Idecabtagene-Vicleucel

Hiroyuki Takamatsu, MD, PhD
Professor
Faculty of Transdisciplinary Sciences, Institute of Transdisciplinary Sciences, Kanazawa University
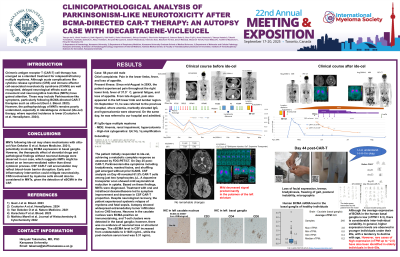
Introduction: Chimeric antigen receptor T (CAR-T) cell therapy has emerged as a standard treatment for relapsed/refractory multiple myeloma. Although acute complications like cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) are well recognized, delayed neurological effects such as movement and neurocognitive toxicities (MNTs) have gained attention. These may include Parkinsonism-like symptoms, particularly following BCMA-directed CAR-T therapies such as cilta-cel (Gust J. Blood. 2023). However, the pathophysiology of MNTs remains poorly understood, especially in idecabtagene vicleucel (ide-cel) therapy, where reported incidence is lower (Couturier A et al. HemaSphere. 2024).
Methods: We report the clinical course and autopsy findings of a 58-year-old Japanese male with triple-class refractory IgG-κ multiple myeloma harboring t(4;14) and 1q gain. Following lymphodepletion, he received ide-cel therapy. We evaluated the patient's neurological symptoms, imaging, CSF analysis including CAR-T cell proportion and soluble BCMA (sBCMA) levels in serum and cerebrospinal fluid (CSF), and conducted postmortem brain histopathology and immunostaining.
Results:
The patient initially responded to ide-cel, achieving a metabolic complete response as assessed by FDG-PET/CT. On Day 25, Parkinsonism-like symptoms including bradykinesia, masked facies, and shuffling gait emerged without prior ICANS. CSF analysis on Day 40 revealed 61.5% CAR-T cells among just two lymphocytes /μL. A dopamine transporter scan showed mild asymmetrical reduction in uptake. Based on these findings, MNTs were diagnosed. Treatment with oral and intrathecal dexamethasone led to symptom improvement and decrease in CSF CAR-T proportion. Despite neurological recovery, the patient experienced systemic relapse of myeloma and fatal sepsis. Autopsy showed widespread extramedullary tumor infiltration but no CNS lesions. The nerve cells in caudate nucleus were BCMA-positive on immunostaining, yet no neuronal loss or structural damage was evident. The sBCMA level in CSF increased from undetectable to 0.1025 ng/mL, while the post-mortem serum level was 5.31 ng/mL.
Conclusions:
MNTs following ide-cel may share mechanisms with cilta-cel (Van Oekelen O et al. Nature Medicine. 2021), potentially involving BCMA expression in basal ganglia. However, the therapeutic effect of steroidal drugs and pathological findings without neuronal damage were observed in our case, which suggests NMTs might be based on an immune-mediated rather than direct cytotoxic process. CSF CAR-T cell accumulation may reflect blood–brain barrier disruption. Early anti-inflammatory intervention could mitigate neurotoxicity. CNS involvement by myeloma cells should also be considered in MNTs, given the detection of sBCMA in the CSF.
