Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
Optimizing CAR-T Therapy in Multiple Myeloma: Outpatient Reinfusion of Cesnicabtagene Autoleucel (ARI0002h)
(PA-072) Optimizing CAR-T Therapy in Multiple Myeloma: Outpatient Reinfusion of Cesnicabtagene Autoleucel (ARI0002h)

Beatriz Merchán Muñoz, Dr (she/her/hers)
Hematologist
Hospital Clinic Barcelona
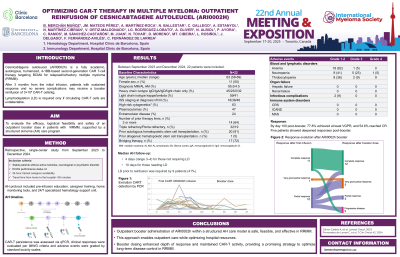
Cesnicabtagene autoleucel (ARI0002h) is a fully academic, autologous, humanized, 4-1BB-based second-generation CAR T-cell therapy targeting BCMA for relapsed/refractory multiple myeloma (RRMM). After 3 months from the initial infusion, patients with sustained response and no severe complications may receive a second infusion of 3×10⁶ CAR-T cells/kg. Lymphodepletion (LD) is required only if circulating CAR-T cells are undetectable. We evaluated efficacy, safety and logistical feasibility of an outpatient booster dose supported by a structured at-home (AH) care program.
Methods:
This retrospective study included 22 RRMM patients who had received initial ARI0002h infusion and met clinical/logistical criteria for outpatient reinfusion, between September 2023 and December 2024. Eligibility included ECOG≤2, no active infection or severe organ comorbidities and availability of a trained 24-hour caregiver. AH protocol included pre-infusion education, caregiver training, home monitoring tools, and 24/7 specialized hematology support unit. Home LD was administered as needed. Vital signs and immune effector cell-associated encephalopathy score were monitored by nursing staff via telephone every 12 hours, with lab tests on days 1 and 3 post-infusion. CAR-T persistence was assessed via qPCR and clinical responses by IMWG criteria.
Results:
Median age was 63 years (range, 49-75). Most patients (95.4%) had MM, and one had AL amyloidosis. At baseline, 80% had ISS II/III, 63.1% high-risk cytogenetics and 23.8% extramedullary disease. All patients had received ≥2 prior therapies, 31.8% were triple-refractory and 18.2% penta-refractory. Before first CART infusion, bridging therapy was used in 77.2%, mainly cyclophosphamide-based regimens (41.1%). LD was administered in 40.9% before reinfusion. AH follow-up was 4 days (range, 3–4) for those not requiring LD, and 10 days for those needing LD. No patients developed cytokine release syndrome, immune effector cell-associated neurotoxicity syndrome or macrophage activation syndrome after booster infusion. CAR-T re-expansion was observed in 72.7% of patients, more frequently in LD recipients (88.9% vs. 61.5%, p=0.157). By day 100 post-booster, 77.8% achieved at least VGPR, and 54.6% reached CR. Five patients (22.7%) showed deepened responses post-booster: 2 patients in partial response achieved CR, and 3 patients improved to VGPR. Eighteen patients (81.1%) remain in response, while only 4 patients (18.2%) experienced disease progression after a median of 7 months (IQR 6–10). No patient required hospitalization within 45 days of booster; no treatment-related secondary malignancies have been reported.
Conclusions:
Outpatient second administration of ARI0002h within a structured AH care model is safe, feasible, and effective in RRMM. This approach enables outpatient care while optimizing hospital resources. Second infusions enhanced depth of response and maintained CAR-T activity, providing a promising strategy to optimize long-term disease control in RRMM.
