Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
An evaluation of overall survival between B-cell maturation antigen chimeric antigen receptor T cell therapies and bispecific antibodies for the treatment of relapsed/refractory multiple myeloma
(PA-070) An Evaluation of Overall Survival Between B-cell Maturation Antigen Chimeric Antigen Receptor T Cell Therapies and Bispecific Antibodies for the Treatment of Relapsed/refractory Multiple Myeloma

Noopur Raje, MD
Director, Multiple Myeloma Program, Professor of Medicine
Center for Multiple Myeloma, Massachusetts General Hospital, Harvard Medical School
Introduction:
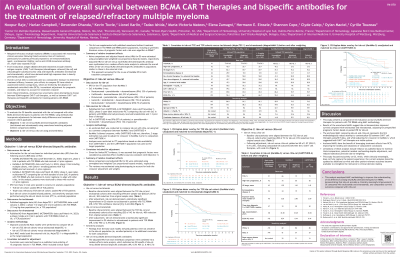
B-cell maturation antigen (BCMA) chimeric antigen receptor (CAR) T cell therapies (idecabtagene vicleucel [ide-cel] and ciltacabtagene autoleucel [cilta-cel]) and bispecific antibodies (teclistamab and elranatamab) have not been directly or indirectly compared in a methodologically robust manner. Previous indirect comparisons between CAR T cell therapies were unanchored, did not incorporate randomized controlled trial (RCT) evidence, and did not adjust for crossover in KarMMa-3 overall survival (OS). This study aimed to compare OS across BCMA CAR T cell therapies and bispecific antibodies for the treatment of patients with relapsed/refractory multiple myeloma (RRMM).
Methods:
Objective 1: Individual-level patient data (IPD) for ide-cel were pooled across KarMMa (phase 2), KarMMa-2 (phase 2), and KarMMa-3 (phase 3; ≥ 4 prior lines) to form triple-class exposed (TCE) and triple-class refractory (TCR) cohorts. The ide-cel TCE cohort was compared with aggregate data (AD) for teclistamab 1.5 mg/kg population (phase 2 MajesTEC-1; 100% TCE), and the ide-cel TCR cohort was compared with AD for elranatamab cohort A (MagnetisMM-3; 100% TCR). Unanchored matching-adjusted indirect comparisons (MAICs) were performed adjusting for prespecified 9 to 11 prognostic factors and/or effect modifiers across analyses, targeting each external trial. Objective 2: IPD from KarMMa-3 (intent-to-treat [ITT] population) was compared with AD from cilta-cel (phase 3 CARTITUDE-4; ITT population) using an anchored MAIC to target a population similar to CARTITUDE-4, assuming that standard of care (SoC) between the RCTs was comparable. OS from KarMMa-3 was adjusted for crossover using the 2-stage estimation. Seven prespecified effect modifiers were adjusted for in the analysis.
Results:
For the interclass unanchored MAICs, 368 pooled ide-cel TCE patients were compared with 165 teclistamab patients (effective sample size [ESS] 235), and 272 pooled ide-cel TCR patients were compared with 123 elranatamab patients (ESS 142). Ide-cel was associated with improved OS versus teclistamab (hazard ratio [HR], 0.59; 95% confidence interval [CI], 0.44–0.80) and elranatamab (HR, 0.58; 95% CI, 0.39–0.86). For the intraclass anchored MAIC, 254 ide-cel and 132 SoC patients from KarMMa-3 were compared with 208 cilta-cel and 211 SoC patients from CARTITUDE-4, resulting in an ESS of 73 (48 for ide-cel and 25 for SoC). Ide-cel and cilta-cel had comparable OS benefits (HR, 1.07; 95% CI, 0.41–2.81), with wide CIs. This analysis reflects the first anchored comparison of ide-cel and cilta-cel incorporating RCT evidence and crossover adjustment.
Conclusions:
This analysis demonstrates that ide-cel provides a clinically meaningful improvement in OS for patients with RRMM compared with teclistamab and elranatamab (BCMA-directed antibodies) and offers comparable survival outcomes to cilta-cel (BCMA-directed CAR T cell therapy).
