Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
INFECTIONS IN PATIENTS (PTS) WITH MULTIPLE MYELOMA (MM) TREATED WITH BCMA-DIRECTED CAR T CELL THERAPIES AND BISPECIFIC ANTIBODIES: ANALYSIS OF THE FDA ADVERSE EVENT REPORTING SYSTEM (FAERS)
(PA-067) Infections in Patients (PTS) with Multiple Myeloma (MM) Treated with BCMA-directed Car T Cell Therapies and Bispecific Antibodies: Analysis of the FDA Adverse Event Reporting System (FAERS)

Surbhi Sidana, MD
Associate Professor
Stanford University School of Medicine
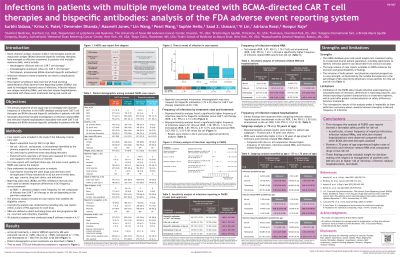
Novel B-cell maturation antigen (BCMA)-directed therapies including chimeric antigen receptor (CAR) T cells (idecabtagene vicleucel [ide-cel], ciltacabtagene autoleucel [cilta-cel]) and bispecific antibodies (teclistamab, elranatamab) have emerged as effective treatments for MM. FAERS is a real-world (RW) post-marketing safety surveillance database capturing adverse events (AEs) reported to the US FDA for all marketed drugs and biologics across a broad population. We assessed RW infection-related AEs in pts receiving BCMA-directed CAR T cells and bispecific antibodies using FAERS.
Methods:
We used FAERS to capture infections and infection-related non-relapse mortality (NRM) and hospitalizations from case report forms (CRFs) in pts with MM where ide-cel, cilta-cel, teclistamab, or elranatamab were identified as drugs of interest. Infection-related NRM was defined as deaths excluding any from progressive MM with further filtering for infections. Infection-related hospitalization was defined similarly. The primary analysis used all CRFs from Q1 2021 to Q4 2024, the latest FAERS quarterly release. To adjust for differences in follow-up duration between treatments after market approval, we conducted sensitivity analyses by restricting the CRF analysis time to 2 y post-market approval for each drug.
Reporting odds ratios (ROR) were used to identify differences between treatments; a ROR >1 indicates the event was reported more frequently for the comparator than ide-cel.
Results:
Overall, 4809 AE reports in MM were associated with ide-cel (n=689), teclistamab (n=1732), elranatamab (n=363), and cilta-cel (n=2025).
In disproportionality analyses (ROR [95% CI]), a significantly higher frequency of infection reports was associated with teclistamab (3.81 [2.51–5.77]), elranatamab (5.67 [3.53–9.10]), and cilta-cel (1.78 [1.16–2.73]) vs ide-cel. Results were similar in sensitivity analyses.
Teclistamab (ROR, 4.02 [95% CI, 1.43–11.32]) and elranatamab (ROR, 5.57 [95% CI, 1.76–17.65]) had a significantly higher frequency of infection-related NRM reports than ide-cel. Results were comparable between ide-cel and cilta-cel (ROR, 1.01 [95% CI, 0.33–3.12]). Similar findings were observed for infection-related hospitalizations (teclistamab: ROR, 3.44 [95% CI, 2.03–5.83]; elranatamab: ROR, 5.65 [95% CI 3.14–10.19]; and (cilta-cel: ROR, 1.53 [95% CI, 0.88–2.65]).
Conclusions:
FAERS provides long-term follow-up data of drug safety, offering insights beyond pts meeting clinical trial criteria and providing greater statistical power to identify and understand observed toxicities. This retrospective analysis showed a favorable RW safety profile for ide-cel vs other BCMA-directed therapies in terms of infections and infection-related NRMs and hospitalizations. This highlights the importance of integrating safety profiles into treatment decisions to optimize outcomes and reduce risks, especially infection-related burden and mortality in pts with MM who are immunocompromised or have other comorbidities.
