Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
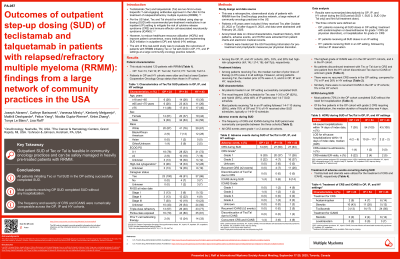
Outcomes of outpatient step-up dosing (SUD) of teclistamab and talquetamab in patients with relapsed/refractory multiple myeloma (RRMM): findings from a large network of community practices in the USA
(PA-057) Outcomes of Outpatient Step-up Dosing (SUD) of Teclistamab and Talquetamab in Patients with Relapsed/refractory Multiple Myeloma (RRMM): Findings from a Large Network of Community Practices in the USA
- LR
Lisa Raff, PharmD
Vice President of Pharmacy Services
OneOncology
Teclistamab (Tec) and talquetamab (Tal), two first-in-class bispecific T-cell engaging antibodies approved for the treatment of RRMM, should be initiated using SUD in an inpatient (IP) setting to mitigate the risk of cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS), per US label. However, to reduce IP healthcare resource utilization and improve patient (pt) experience, outpatient (OP) [OP SUD with acetaminophen or dexamethasone for Grade 1 CRS, or hospitalization for Grade 2+ CRS] and hybrid (HY) SUD [OP SUD with 48 h IP observation] is also being implemented. This real-world study evaluated the outcomes in pts with RRMM initiating Tec or Tal with SUD in OP, HY, and IP settings.
Methods:
This was a retrospective, observational, three-cohort (SUD in IP, OP, and HY settings) study of pts with RRMM (≥18 years) from a large network of community oncology practices in the US. Anonymized data on clinical characteristics, adverse events (AEs), and treatment history for pts initiating Tec (from Oct 2022) or Tal (from Aug 2023) were extracted till Feb 2025 from EMR for the first 14 days of SUD. Descriptive results were analysed for all cohorts.
Results:
This study included 120 pts with RRMM (OP: Tec=13, Tal=10; IP: Tec=42, Tal=12; HY: Tec=29, Tal=14), of which 48%, 40%, and 31% were aged ≥75 years in the OP, HY, and IP cohorts, respectively. Among the OP, IP, and HY cohorts, 9%, 13%, and 28% of pts were Black; 9%, 19%, and 17% had ECOG scores of ≥2; and 26%, 33%, and 28% had high-risk cytogenetics (t(4; 14); t (14; 16); del17p), respectively. Most pts were penta-drug exposed (OP=70%, IP=80%, HY=81%). Tec and Tal pts had 4 median prior lines of therapy (PL) in OP, 4 and 5 PLs in IP, and 4 and 6 PLs in HY, respectively. More pts in IP (24%) and HY (33%) cohorts had prior exposure to T-cell redirecting therapy than the OP cohort (9%). The most frequent OP SUD schedule was 1-3-5 (62%) for pts receiving Tec. Most Tal pts followed biweekly dosing (80%). The 14-day CRS rates were comparable across cohorts (OP=61%, IP=50%, HY=63%); the highest grade (G) of CRS was 2 (OP=22%, IP=7%, HY=37%). Pts received tocilizumab for the treatment of CRS (OP=13%, IP=17%, HY=56%). No pts discontinued treatment due to CRS. All OP Tec and Tal pts successfully completed SUD, with G2 CRS patients needing 4 days (median) of hospitalization. The 14-day frequency of ICANS was low (OP: G2=4%, IP: G1=2%, G2=2%, G4=2%, HY: G1=9%, G2=2%, unknown=2%). Pts received steroids for the treatment of ICANS (OP=0%, IP=4%, HY=14%). No pts were hospitalized due to ICANS. One pt from HY cohort discontinued treatment due to ICANS. Most OP pts completed SUD without the need for hospitalization (70%).
Conclusions:
In community oncology practices, OP SUD showed comparable rates and severity of CRS and ICANS as IP/HY SUD. OP SUD of Tec or Tal is feasible and can be safely managed in heavily pre-treated pts with some requiring hospitalization for G2 CRS.
