Myeloma Genomics and Microenvironment and immune profiling
Category: Myeloma Genomics and Microenvironment and immune profiling
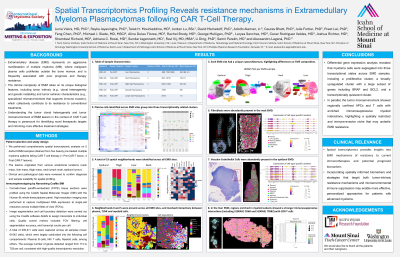
Spatial Transcriptomics Profiling Reveals resistance mechanisms in Extramedullary Myeloma Plasmacytomas following CAR T-Cell Therapy
(PA-270) Spatial Transcriptomics Profiling Reveals Resistance Mechanisms in Extramedullary Myeloma Plasmacytomas Following CAR T-cell Therapy

Alessandro Lagana, PhD
Assistant Professor
Icahn School of Medicine at Mount Sinai
Methods: We performed comprehensive spatial transcriptomic analysis on 5 distinct EMM samples obtained from five heavily pre-treated multiple myeloma patients failing CAR T-cell therapy (1 Pre-CAR-T lesion, 4 Post-CAR-T lesions). The lesions originated from various anatomical locations (neck mass, liver mass, thigh mass, neck lymph node, epidural tumor). All samples underwent spatial profiling using the CosMx SMI 6k panel. Downstream analysis was performed on selected high quality FOVs from each EMM sample.
Results:
The total number of cells detected on each EMM sample ranged from 20,154 cells to 155,648 cells (mean 61042 cells, total cells 305211), which were largely subdivided into the following cell compartments: Plasma/ B cells, NK/ T cells, Myeloid cells, among others. The average number of genes detected ranged from 114 to 729 genes/cell.
Differentially expressed genes derived from sample specific myeloma cell clusters were classified into 3 transcriptional groups and present across multiple samples. Two clusters were more transcriptionally active, one contained a proliferative signature (MKI67, HMGB2, STMN1) while the other upregulated a larger subset of genes (BRAF, BCL2), and a third transcriptionally quiescent cluster.
Within the tumor microenvironment, we observed regional confinement of antigen-presenting cells (APCs) and T cells in all EMM samples. Notably, in the liver EMM sample, this confinement was particularly striking, with APCs and CD8 T cells restricted to a small region while over 80% of the tumor consisted of myeloma cells, indicating a generally poor immune infiltrate. Cell communication analysis revealed enrichment of immunosuppressive interactions of myeloid cells amongst themselves (S100A9/CD68 and S100A9/ITGB2) and with CD8 T cells (S100A9/ITGB2 and B2M/KLRD1). These interactions can potentially disturb Myeloid and T cell trafficking to other tumor regions, contributing to the formation of an immunosuppressive microenvironment in EMM.
Conclusions: Spatial transcriptomics of EMM reveals pronounced inter- and intra-tumoral heterogeneity in both clonal architecture and immune microenvironments. The identification of highly proliferative tumor cells along with immune deserts, spatially restricted T cell/APC niches, and immunosuppressive signaling circuits highlights critical barriers to effective immune surveillance in EMM. These findings underscore the importance of tissue-specific microenvironmental contexts in shaping therapeutic response and provide a rationale for incorporating spatially informed biomarkers and combinatorial immune-modulating strategies in the treatment of EMM.
