Myeloma Genomics and Microenvironment and immune profiling
Category: Myeloma Genomics and Microenvironment and immune profiling
Single-Cell Transcriptomic Stratification of Multiple Myeloma Reveals Oxidative Stress-Driven Subtypes and Cytogenetic Correlates
(PA-213) Single-Cell Transcriptomic Stratification of Multiple Myeloma Reveals Oxidative Stress-Driven Subtypes and Cytogenetic Correlates

Marta Biondo, PhD
Postdoctoral Researcher
Division of Haematology, Azienda Ospedaliera Policlinico-Vittorio Emanuele, University of Catania, Catania, Italy,
Multiple myeloma (MM) is a plasma cell malignancy characterized by bone marrow infiltration and high genomic instability. Clonal plasma cells (cPCs) in MM exhibit elevated oxidative stress (OS) due to intense metabolic activity and protein synthesis, resulting in the production of reactive oxygen species (ROS). To survive, these cells rely on antioxidant systems such as superoxide dismutase (SOD), glutathione peroxidase (GPX), and thioredoxin reductase (TrxR). Upregulation of these pathways has been linked to drug resistance and poor prognosis.
We aimed to define OS-related molecular subtypes of MM by analyzing a large collection of single-cell transcriptomic profiles, with the goal of uncovering stress-linked vulnerabilities and identifying immune and genetic correlates of malignant plasma cell states.
Methods:
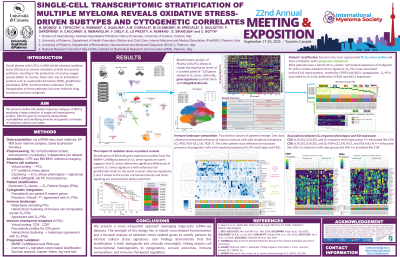
We integrated raw scRNA-seq data from 10 publicly available GEO datasets (n = 64 patients), extracting 93,071 bone marrow plasma cell profiles. Data underwent individual quality control, normalization, and reference-based annotation. A curated panel of 210 OS-related genes was used to cluster cells via PCA, UMAP, and the Leiden algorithm. This revealed seven OS-related clusters (O2_clusters) reflecting distinct transcriptional stress signatures.
Patients were assigned to O2_clusters based on the dominant stress phenotype in their plasma cells. We created pseudobulk profiles for each patient to assess expression of genes linked to major cytogenetic events in MM (FGFR3, CCND1, MCL1, etc.), allowing cytogenetic stratification. The complete cellular dataset was also used to evaluate immune cell-type differences between O2_clusters.
Results:
Seven transcriptionally distinct O2_clusters were identified. 52 patients showed a dominant plasma cell cluster, suggesting monoclonality of the OS phenotype. O2_cluster_1 was associated with t(4;14) translocations, marked by FGFR3 and MCL1 upregulation. O2_cluster_2 was linked to t(11;14), defined by CCND1 and MCL1 expression. Other clusters revealed potentially novel cytogenetic states.
Immune landscape analysis showed cluster-specific traits with distinct profiles across O2_clusters. O2_cluster_1_ t(4;14) patients had increased Prog-B cell fractions and reduced MAIT. O2_cluster_2_ t(11;14) showed lower cDC2 and pDC content. O2_cluster_3, marked by chaperones like CCT3 and BAG1, had elevated Naive B cells. O2_cluster_4 exhibited enrichment in Memory B, Lymphoid-Primed Multipotent Progenitors.
Conclusions:
This study introduces a scalable bioinformatics pipeline for MM patient stratification based on OS-related transcriptional programs. Cross-cohort integration of scRNA-seq data revealed distinct stress-driven plasma cell subtypes with specific genetic and immune correlates. These findings highlight the utility of large-scale single-cell analyses for identifying clinically relevant MM biomarkers and stress-related therapeutic targets, underscoring the potential of bioinformatics in precision oncology.
