Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
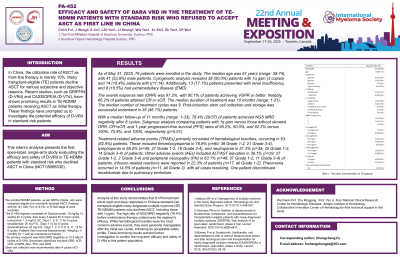
Interim Analysis of DARA VRD in the Treatment of TE-NDMM Patients with Standard Risk Who Refused to Accept ASCT as First Line in China
(PA-452) Interim Analysis of DARA VRD in the Treatment of TE-NDMM Patients with Standard Risk Who Refused to Accept ASCT as First Line in China
.jpg)
Chengcheng FU
Chief Physician
The First Affiliated Hospital of Soochow University, Suzhou, PRC
In China, ASCT as front-line therapy is merely 10%. Studies, such as GRIFFIN (D-VRd) and CASSIOPEIA (D-VTd), have shown promising results in TE-NDMM patients receiving ASCT as initial therapy.These findings have prompted us to investigate the potential efficacy of D-VRd in standard-risk patients.This interim analysis presents the first open-label, single-arm study evaluating the efficacy and safety of D-VRd in TE-NDMM patients with standard risk who declined ASCT in China (NCT 05088330).
Methods:
We enrolled IMWG-defined NDMM patients,who were TE but voluntarily declined ASCT,excluding those with t(4;14), Del(17p), t(14;16), R-ISS stage III.The D-VRd regimen consisted:Daratumumab:16 mg/kg I.V. weekly for 2 cycles, then every 3 weeks for 6 more cycles,bortezomib:1.3 mg/m2 SC,Days 1, 4, 8, 11,lenalidomide:25 mg P.O.,Days 1-14,dexamethasone:20 mg P.O.,Days 1, 2, 4, 5, 8, 9, 11, 12.All for 8 cycles, followed by daratumumab maintenance:16mg/kg q4w×12mo.The primary endpoint was NGS MRD negativity at 10-5 after 8 cycles of D-VRd.Secondary objectives included ORR,sCR,≥CR,≥VGPR, AEs,TTR, and DOR.Stem cell collection advised post-Cycle 4.
Results:
By June 30, 2024, 46 pts were enrolled.The median age was 62 years, with 23 male pts. Cytogenetic analysis revealed 27 patients with 1q gain and 4 pts with t(11;14). Additionally, 8 pts presented with renal insufficiency, and 6 had EMD. The ORR was 97.4%, with 89.7% of pts achieving VGPR or better. Notably, 64.1% of patients attained CR or sCR. The median treatment duration was 10 months and median treatment cycles was 9.19 pts successfully underwent autologous stem cell collection and storage. With a median follow-up of 12 months, 72.7% of pts achieved NGS MRD negativity after 8 cycles. Subgroup analysis comparing pts with 1q gain versus those without showed ORR, CR+sCR, and 1-year progression-free survival rates of 95.8%, 58.3%, and 88.2% versus 100%, 73.3%, and 100%, respectively (p >0.01). Treatment-related adverse events primarily consisted of hematological toxicities, occurring in all 46 pts.These included thrombocytopenia in 80.4% (n=37; 22 Grade 1-2, 15 Grade 3-4), lymphopenia in 58.7% (n=27; 17 Grade 1-2, 10 Grade 3-4), and neutropenia in 43.4% (n=20;9 Grade 1-2, 11Grade 3-4) of pts. Other adverse events included ALT/AST elevation in 43.4% (n=20; 19 Grade 1-2, 1 Grade 3-4) and peripheral neuropathy in 45.7% (n=21;12 Grade 1-2, 9 Grade 3-4) of pts. Infusion-related reactions were reported in 23.9% of pts (n=11,all Grade 1-2). Pneumonia occurred in 13.0% of pts (n=6,all Grade 3),with all cases resolving.One patient discontinued lenalidomide due to pulmonary embolism.
Conclusions: Interim analysis shows D-VRd induces rapid, deep responses in Chinese TE-NDMM patients declining ASCT (including1q gain). High NGS MRD negativity (72.7%) pre-maintenance underscores efficacy. Hematological toxicities (most common AEs) were manageable after cycle 2, supporting acceptable safety.These results warrant further long-term evaluation.
