Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Evaluation of haematopoietic second primary malignancies in multiple myeloma: a single centre Australian experience
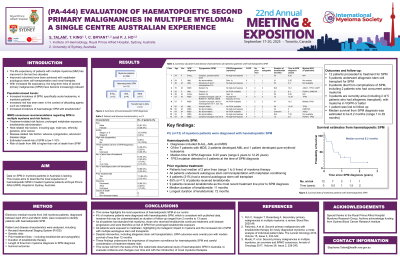
(PA-444) Evaluation of Haematopoietic Second Primary Malignancies in Multiple Myeloma: A Single Centre Australian Experience

Stephanie Talam, MBBS FRACP FRCPA
Post-Graduate Fellow in Haematology (Myeloma)
Royal Prince Alfred Hospital
Novel myeloma therapies have led to increased life expectancy. Long-term risk of second primary malignancies (SPM) has become increasingly relevant. Increased risk has been seen in the context of alkylating agents, such as melphalan, and lenalidomide. Data on SPM in myeloma patients in Australia is lacking. This study describes the local experience of haematopoietic SPM in treated myeloma patients at Royal Prince Alfred Hospital in Sydney, Australia.
Methods:
Electronic medical records from 346 myeloma patients, diagnosed from April 2012 to March 2025, were reviewed to identify patients with haematopoietic SPM. Patient and disease characteristics were analysed, including prior treatment lines and autograft(s), genetic risks, duration of lenalidomide and survival outcomes.
Results:
13 patients were identified with haematopoietic SPM: B-cell acute lymphoblastic leukaemia (n=2), acute myeloid leukaemia (n=4), myelodysplastic neoplasm (n=7). Of 7 patients with MDS, 1 developed AML. 5 patients had mutated TP53 at the time of SPM diagnosis. In myeloma FISH analysis, 2 patients had gain of 1q with no other high-risk cytogenetic abnormalities. 11 patients did not have high-risk cytogenetic features, or results were unavailable. All patients underwent autologous stem cell transplantation for myeloma; 4 patients had a second autograft at the time of disease progression. 11 patients received lenalidomide, of whom 9 received lenalidomide as the most recent line of treatment prior to SPM diagnosis. Median duration of lenalidomide was 33 months and longest duration was 72 months. All patients had standard risk myeloma and were at risk of SPM from prolonged lenalidomide. Median time to SPM diagnosis was 6.25 years. 4 patients are currently alive. 1 patient had non-SPM-related death. Median survival time is 9.6 months.
Table 1. Summary of patient and disease characteristics for myeloma patients with haematopoietic SPM
Age | Sex | SPM diagnosis | FISH/Cytogenetics (myeloma) | R-ISS | No. prior treatment lines | No. autografts | Duration of lenalidomide (months) | Myeloid NGS |
54 | F | B-ALL | No high-risk features | I | 1 | 1 | 35 | N/A |
54 | F | AML | Gain 1q | II | 1 | 1 | 31 | No variants |
46 | M | AML | No high-risk features | I | 1 | 1 | 23 | Not available |
76 | M | MDS | No high-risk features | II | 3 | 2 | N/A | ASXL1, TP53, U2AF1 |
59 | F | AML | No FISH available | I | 2 | 1 | 31 | RUNX1, DNMT3A |
69 | M | B-ALL | Gain 1q | I | 1 | 1 | 55 | N/A |
57 | M | MDS | t(11;14) - No high-risk features | II | 5 | 2 | 72 | TP53 |
67 | F | MDS | No FISH available | I | 2 | 2 | 47 | Biallelic TP53 |
65 | M | AML | No FISH available | I | 2 | 2 | 56 | TP53 |
65 | M | MDS | No high-risk features | I | 2 | 1 | 23 | DNMT3A |
64 | M | MDS | Unknown | I | 1 | 1 | Unknown | ASXL1 |
52 | F | MDS | No high-risk features | II | 1 | 1 | N/A | Not available |
54 | M | MDS | No high-risk features | II | 4 | 1 | 12 | RUNX1, TP53 |
Conclusions:
This review highlights the experience of haematopoietic SPM at our centre, with diagnoses including B-ALL, AML and MDS. This review will form the basis of the first nationwide observational study of haematopoietic SPM in Australia, to evaluate incidence over time and with the introduction of novel myeloma therapies.
