Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
TREATMENT ACCESSIBILITY, AVAILABILITY, AND HEALTHCARE COSTS FOR MULTIPLE MYELOMA IN SOUTH ASIAN COUNTRIES
(PA-421) Treatment Accessibility, Availability, and Healthcare Costs for Multiple Myeloma in South Asian Countries

Roopika R L Peela, Final MBBS student (she/her/hers)
Student
Armed Forces Medical College
Introduction:
Regional disparities in multiple myeloma (MM) care is leading to variable outcomes in South Asia. This study assesses the availability, accessibility, and cost of MM treatments in South Asian countries to identify gaps in care and inform healthcare policy.
Methods:
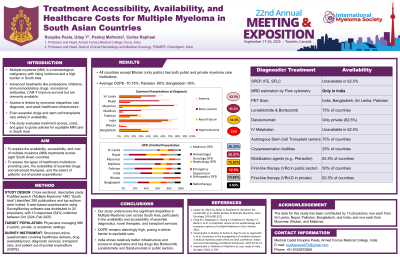
A cross-sectional, descriptive study was conducted through a web-based survey targeting physicians managing MM patients in Bangladesh, Bhutan, India, Maldives, Myanmar, Nepal, Pakistan and Sri Lanka. The survey covered institutional healthcare structures, drug availability, treatment regimens, diagnostic access, and patient out-of-pocket expenditures (OOPE). Data were analyzed to evaluate disparities in MM care across public and private healthcare sectors.
Results:
Public and private healthcare institutions coexist in all studied countries except Bhutan, where MM care is primarily public. Physicians reported a high OOPE for MM treatment, with patients covering an average of 70% of total medical costs. Key diagnostic investigations such as serum protein electrophoresis, immunofixation, and free light chain assays, were unavailable in public hospitals in 62.5% of the countries, while minimal residual disease estimation via flow cytometry was available publicly only in India. PET scans were available in public hospitals in India, Bangladesh, Sri Lanka and Pakistan but remained cost prohibitive. Lenalidomide and bortezomib were available in public institutions in 75% of the countries, while advanced therapies like daratumumab were largely restricted to private institutions in 62.5% of the countries. IV melphalan was unavailable in public institutions in 62.5% of the countries. Autologous stem cell transplant (ASCT) centers were reported in 75% of the studied countries; however, cryopreservation facilities were limited to 25% of the countries, and mobilization agents like plerixafor were accessible in 62.5% countries. The most commonly used first-line therapy for transplant-eligible patients in public institutions was VRd (bortezomib, lenalidomide, dexamethasone) in 50% of the countries, while private institutions more frequently incorporated daratumumab (VRd-D). Only India had a dedicated myeloma patient support group, whereas general oncology support groups were reported in 62.5% of the countries.
Conclusions:
There are significant disparities in MM treatment accessibility across South Asia. Public sector institutions often lack essential diagnostic tools and advanced therapies, forcing patients to rely on private healthcare at high OPE. Improved government policies, financial assistance programs, and public-private partnerships are needed to enhance drug accessibility, diagnostic infrastructure, and transplant availability.
