Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Daratumumab-based salvage treatment for multiple myeloma: experience from a Peruvian institution .
(PA-519) Daratumumab-based Salvage Treatment for Multiple Myeloma: Experience from a Peruvian Institution

Jule Vasquez, MD (he/him/his)
Oncologist
AUNA
Introduction:
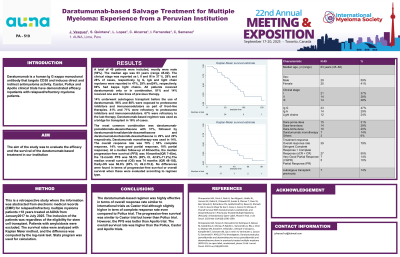
Daratumumab is a human IgGκ monoclonal antibody that targets CD38 and induces direct and indirect antimyeloma activity. Castor, Pollux and Apollo clinical trials have demonstrated efficacy in patients with relapsed/refractory myeloma patients. The aim of the study was to evaluate the efficacy and the survival of the daratumumab-based treatment in our institution
Methods:
This is a retrospective study where the information was abstracted from electronic medical records (EMR) for relapsed/refractory multiple myeloma patients >18 years treated at AUNA from January 2017 to July 2025. The inclusion of the patients was regardless of the eligibility for stem cell transplant. Patients with amyloidosis were excluded. The survival rates were analyzed with Kaplan Meier method and the difference was computed by the log-rank test. Stata program was used for calculation.
Results:
A total of 49 patients were included, mostly were male (59%). The median age was 63 years (range 45-82). The clinical stage was reported as I, II and III in 37 %, 28% and 28% of cases, respectively. Ig G, IgA and light chain myeloma were reported in 47%, 29% and 24%, respectively. 69% had kappa light chains. All patients received daratumumab only or in combination. 81% and 14% received one and two lines of previous therapy. 14% underwent autologous transplant before the use of daratumumab. 96% and 88% were exposed to proteosome inhibitors and immunomodulators as part of front-line therapies. 41% and 71% were refractory to proteosome inhibitors and immunomodulators. 67% were refractory to the last therapy. Daratumumab-based regimen was used as a bridge for transplant in 16% of cases. The most common combination was daratumumab-pomalidomide-dexamethasone with 31%, followed by daratumumab-lenalidomide-dexamethasone and daratumumab-bortezomib-dexamethasone in 29% and 20% respectively. Daratumumab monotherapy was used in 14%. The overall response rate was 79% ( 55% complete response, 14% very good partial response, 10% partial response). At a median follow-up of 48 months, the median progression-free survival (PFS) was 16months (IQR 7-45m), the 12-month PFS was 58.5% (95% CI, 42.9%-71.2%). The median overall survival (OS) was 74 months (IQR 48-102), the 5y-OS was 66.6% (95% CI, 49.2-79.2). No differences were found in terms of progression-free survival or overall survival when these were evaluated according to regimen type.
Conclusions:
The daratumumab-based regimen was highly effective in terms of overall response rate similar to international trials as Castor trial although slightly higher in term of complete response rate even compared to Pollux trial. The progression-free survival was similar to Castor trial but lower than Pollux trial. However, the PFS was better than Apollo trial. The overall survival rate was higher than the Pollux, Castor and Apollo trials.
