Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
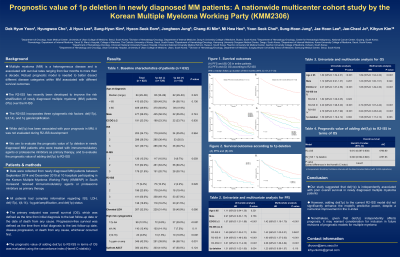
Prognostic Value of 1p Deletion in Newly Diagnosed Multiple Myeloma Patients: A Nationwide Multicenter Cohort Study by the Korean Multiple Myeloma Working Party (KMM2306)
(PA-385) Prognostic Value of 1p Deletion in Newly Diagnosed Multiple Myeloma Patients: A Nationwide Multicenter Cohort Study by the Korean Multiple Myeloma Working Party (KMM2306)

Hyungwoo Cho
Professor
Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine
Introduction:
The Revised Second International Staging System (R2-ISS) was developed to improve risk stratification in patients with newly diagnosed multiple myeloma (MM) beyond the existing R-ISS. It incorporates three cytogenetic abnormalities: del(17p), t(4;14), and 1q gain/amplification. While 1p deletion (del(1p)) has been associated with poor outcomes in MM, it was not evaluated during the development of R2-ISS. This study aims to evaluate the prognostic value of del(1p) in patients with newly diagnosed MM treated with immunomodulatory agents (IMiDs) or proteasome inhibitors (PIs) as primary therapy, and to explore whether incorporating del(1p) into the R2-ISS improves prognostication.
Methods:
We retrospectively analyzed data from 822 patients with newly diagnosed MM between September 2014 and December 2019 who received either IMiDs or PIs as initial therapy. Patients with complete data ISS, LDH, del(17p), t(4;14), 1q gain/amplification, and del(1p) were included. The primary endpoint was overall survival (OS), which was defined as the time from date of diagnosis to the date of death from any cause or last follow-up. The prognostic value of adding del(1p) to R2-ISS in terms of OS was evaluated using the Harrell’s concordance index (C-index).
Results:
The median age was 64 years (range, 29–89), and 477 were male (58.0%). According to the R2-ISS classification: 77 (9.4%) were stage I, 196 (23.8%) stage II, 411 (50.0%) stage III, and 138 (16.8%) stage IV. Del(1p) was detected in 93 patients (11.3%). With a median follow-up of 66.6 months (95% CI: 61.2–71.8), median progression-free survival (PFS) and overall survival (OS) were 29.3 months (95%CI: 27.1–31.4) and 59.1 months (95%CI 59.1–76.8), respectively. Patients with del(1p) had significantly worse PFS and OS compared with those without del(1p), with a median PFS of 25.3 vs. 30.0 months (P = 0.035) and a median OS of 42.5 vs. 69.1 months (P = 0.002). In multivariate analysis adjusted for R2-ISS, age, sex, and Eastern Cooperative Oncology Group Performance Status, del(1p) remained an independent prognostic factor for OS (HR: 1.58, 95% CI: 1.17–2.12, P = 0.003), while the association with PFS showed a non-significant trend toward worse outcome (HR: 1.23, 95% CI: 0.96–1.57, P = 0.110). The C-index for OS with R2-ISS alone was 0.613 (95% CI: 0.587–0.638), which improved to 0.620 (95% CI: 0.592–0.646) with the addition of del(1p), though not statistically significant (P = 0.445).
Conclusions:
Our study demonstrated that del(1p) is an independent adverse prognostic factor for OS in newly diagnosed MM patients. While incorporating del(1p) to the R2-ISS yielded a modest, non-significant improvement in predictive accuracy, its prognostic relevance supports consideration for inclusion in future MM risk stratification models.
