MRD and Biomarkers
Category: MRD and Biomarkers
LIGHT CHAIN ESCAPE IN MULTIPLE MYELOMA: A NOT-SO-UNUSUAL PHENOMENON
(PA-188) Light Chain Escape in Multiple Myeloma: A Not-so-unusual Phenomenon

Laura Rosiñol, Doctor (she/her/hers)
Head of Myeloma Unit
Hospital Clinic de Barcelona
Introduction:
Light chain (LC) escape, traditionally measured by light chain (Bence Jones –BJ-) proteinuria, is a phenomenon that indicates the need for urine monitoring during the follow-up of patients with multiple myeloma (MM). However, 24-hour urinary LC monitoring has some limitations, as it is influenced by renal function, incomplete urine collection, and the presence of intact immunoglobulin in the urine, which interferes with LC measurement in a significant proportion of patients. In contrast, serum free light chains (sFLC) have a higher sensitivity and constitute an early marker of progression. It is estimated that 10% of patients relapse in the form of LC escape. However, since the routine implementation of sFLC measurement, there are few data on its actual frequency. The aim of our study is to describe the frequency of different relapse patterns, including LC escape, in patients with MM after autologous stem cell transplant (ASCT).
Methods:
A retrospective study was conducted in 55 patients diagnosed with MM who relapsed after ASCT performed at our center between 2010 and 2020. Serum monoclonal component (sMC), BJ proteinuria, sFLC, and the presence of plasmacytomas were assessed. Four relapse patterns were established: isolated LC escape, increase in sMC plus BJ proteinuria and/or sFLC, isolated increase in sMC, and oligosecretory relapse. The relapse pattern was analyzed at the first, second, third, and fourth relapses. Patients without BJ or sFLC measurements at the time of relapse, as well as pure light chain myelomas (Bence-Jones myelomas), were excluded from the analysis.
Results:
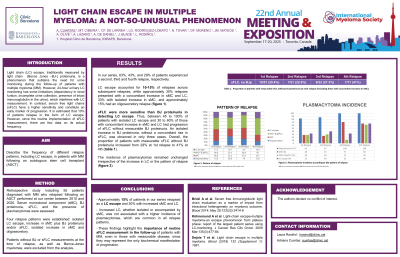
in our series, 63%, 43%, and 29% of patients experienced a second, third, and fourth relapse, respectively. Between 10% and 15% of patients relapsed with LC escape at each successive relapse. Approximately 30% relapsed with concomitant increases in sMC and LC, 33% with isolated increases in sMC, and approximately 15% had an oligosecretory relapse. sFLC were more sensitive than BJ proteinuria in detecting LC escape. Thus, between 45% and 100% of patients with isolated LC escape and 30%-60% of patients with concomitant increases in sMC and LC had progression of sFLC without measurable BJ proteinuria. Overall, the proportion of patients with measurable sFLC without BJ proteinuria increased from 29% at first relapse to 41% at fourth relapse. The incidence of plasmacytomas according to the relapse pattern shows that plasmacytomas are frequent in all patterns, regardless of the increase in LC.
Conclusions:
Approximately 15% of patients in our series relapsed as LC escape, with 30% relapsing with increased sMC and LC. Increased LC, whether isolated or accompanied by sMC, is not associated with an increased incidence of plasmacytomas, which are common in all relapse patterns. These findings underscore the importance of routine sFLC measurement in the follow-up of patients with MM, even in those with measurable disease, since they may represent the only biochemical manifestation of progression.
