Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
High ALC peak post Cilta-Cel infusion predicts risk for delayed neurological toxicities.
(PA-099) High ALC Peak Post Cilta-Cel Infusion Predicts Risk for Delayed Neurological Toxicities

Asya Varshavsky Yanovsky
Associate Professor
Fox Chase Cancer Center
Introduction:
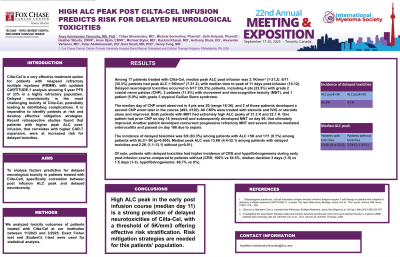
Cilta-Cel is a very effective treatment option for patients with relapsed refractory multiple myeloma (RRMM), with updated CARTITUDE-1 analysis showing 5-year PFS of 33% in a highly refractory population. Delayed neurotoxicity is the most challenging toxicity of Cilta-Cel, potentially leading to debilitating complications. It is imperative to identify patients at risk and develop effective mitigation strategies. Recent retrospective studies found that patients with higher peak ALC post-infusion, that correlates with higher CAR-T expansion, were at increased risk for delayed toxicities.
Methods: We analyzed toxicity outcomes of patients treated with Cilta-Cel at our institution between 11/2023 and 3/2025. Exact Fisher test and Student’s t-test were used for statistical analysis.
Results:
Among 17 patients treated with Cilta-Cel, median peak ALC post infusion was 2.1K/mm3 (1-31.2). I6/17 (35.3%) patients had peak ALC > 5K/mm3 (7-31.2), with median time to peak of 11 days post-infusion (10-12). Delayed neurological toxicities occurred in 6/17 (35.3%) patients, including 4 pts (23.5%) with grade 2 cranial nerve palsies (CNP), 2 pts (11.8%) with movement and neurocognitive toxicity (MNT), and 1 pt (5.9%) with grade 3 atypical Guilian Barre syndrome.
The median day of CNP onset observed in 4 pts was 20 (range 18-36), and 2 of those pateints developed a second CNP event later in the course (d93, d120). All CNPs were treated with steroids and IVIG or steroids alone and improved. Both patients with MNT had extremely high ALC peaks of 31.2 K and 22.1 K. One patient had prior CNP on day 18 (resolved) and subsequently developed MNT on day 66, that ultimately improved. Another patient developed concurrent progressive refractory MNT and severe immune mediated enterocolitis and passed on day 186 due to sepsis.
The incidence of delayed toxicities was 5/6 (83.3%) among patients with ALC >5K and 1/11 (9.1%) among patients with ALC< 5K (p=0.005). Median peak ALC was 13.6K (4.4-32.1) among patients with delayed toxicities and 2.2K (1.1-13.1) without (p=0.01).
Of note, patients with delayed toxicities had higher incidence of CRS and hypofibrinogenemia during early post-infusion course compared to patients without (CRS: 100% vs 54.5%, median duration 3 days (1-5) vs 1.5 days (1-3), hypofibrinogenemia: 66.7% vs 0%).
Conclusions:
High ALC peak in the early post infusion course (median day 11) is a strong predictor of delayed neurotoxicities of Cilta-Cel, with a threshold of 5K/mm3 offering effective risk stratification. Risk mitigation strategies are needed for this patients’ population.
