Imaging, QoL and Patient-Reported Outcome and Supportive Care
Category: Imaging, QoL and Patient-Reported Outcome and Supportive Care
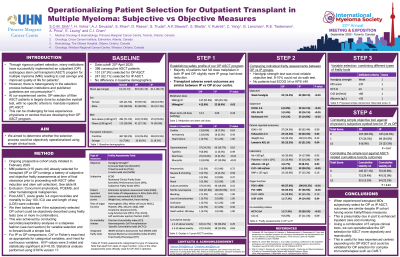
Operationalising patient selection for outpatient transplant in multiple myeloma: Subjective versus objective measures.
(PA-153) Operationalising Patient Selection for Outpatient Transplant in Multiple Myeloma: Subjective versus Objective Measures
Steven Chun-Min Shih, MBChB, FRACP, FRCPA
Haematologist
Cross Cancer Institute
Rigorous patient selection is key to a successful outpatient (OP) autologous stem cell transplant (ASCT) program for myeloma (MM). However, there is heterogeneity in the selection process between institutions. At our experienced centre, OP selection of fitter ASCT patients is largely done by subjective eyeball test, with no specific criteria to mandate inpatient (IP) ASCT. We aimed to determine whether the selection process could be objectively operationalised using simple clinical tools.
Methods:
In a prospective study at our centre, MM patients already selected for transplant (IP or OP) undergo a battery of subjective and objective frailty assessments prior to ASCT: 1) objective measures of fitness [hand grip strength, 6-min walk test, Timed Up and Go, 2) subjective measures of function (Rockwood Frailty, Karnofsky Performance [KPS], ECOG), 3) comorbidity index (HCT-CI), 4) integrative scores (R-MCI, IMWG-GA) and 5) organ function (eGFR, serum albumin, BNP, PFT, ECHO). Post-ASCT, acute grade 3-4 organ toxicities and mortality to Day 100, ICU use and length of stay (LOS) are collected. Apart from tests of organ function, none of the above are used officially for OP ASCT selection. We then looked to see if the subjectively selected OP cohort could objectively be described using frailty tests (one or more in combination). Chi2 or Fisher’s exact test for IP vs OP comparisons were used, as appropriate.
Results:
Of 398 consecutive ASCT patients, 151 (37.9%) were selected for OP at MD discretion. When comparing OP to IP, there were no differences in demographics (age, gender, BMI), severe toxicities, ICU admissions or mortality within 100 days. As expected in this selected ASCT population, no patients had ECOG ≥4 or KPS ≤40. Only 26 (6.5%) received dose-reduced melphalan.
When comparing objective frailty measures between IP and OP, the handgrip test was the most reliable fitness test (11% unable to perform walk-based tests) with weak handgrip in 15.2% OP vs 28.1% IP (p< 0.01). Not surprisingly, the OP group were less likely to have poor KPS ≤70 (p< 0.01), had fewer comorbidities as per HCT-CI ≥4 (p< 0.01), had higher serum albumin (p=0.03) and less renal impairment eGFR < 60ml/min (p< 0.01). Using these 5 selected objective tests, we identified that patients deficient in ≥2 measures had increased risk of ≥2 severe transplant-related toxicities (p=0.03), correlating with IP status, as selected by subjective eyeball method (p< 0.01).
Conclusions:
When experienced transplant MDs subjectively select for OP vs IP ASCT, outcomes (toxicities, ICU use, 100-day mortality) are similar despite the IP cohort having worse frailty/fitness measures. This is presumably due in part to enhanced inpatient care and monitoring. Using a combination of 5 simple clinical tools, we can operationalise the OP selection for ASCT more objectively and reproducibly. This is useful for less experienced centres expanding into OP ASCT and could be validated for OP selection of complex immunotherapies such as CAR-T.
