Imaging, QoL and Patient-Reported Outcome and Supportive Care
Category: Imaging, QoL and Patient-Reported Outcome and Supportive Care
Time Constraints and Treatment Decisions: How Time Allowed for Decision Making Affects Patient Experience in Relapsed Refractory Multiple Myeloma
(PA-113) Time Constraints and Treatment Decisions: How Time Allowed for Decision Making Affects Patient Experience in Relapsed Refractory Multiple Myeloma

Jorge Arturo Hurtado Martinez, MD, MHSc (he/him/his)
Senior Manager, Clinical Research
HealthTree Foundation
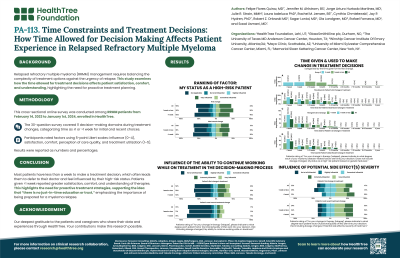
Relapsed-refractory multiple myeloma (RRMM) management requires balancing the complexity of treatment options against the urgency of relapse. This study examines how the time allowed for treatment decisions affects patient satisfaction, comfort, and understanding, highlighting the need for proactive treatment planning.
Methods:
This retrospective, cross-sectional survey included RRMM patients from Feb. 14, 2023, to Jan. 1, 2024, via HealthTree Cure Hub. The 30-question survey covered 11 decision-making domains during treatment changes, categorizing decision-making time as ≤1 week or >1 week for initial and recent treatment choices. Participants rated factors using 5-point Likert scales: influence (0–4), satisfaction, comfort, perception of care quality, and treatment utilization (1–5).
Results:
Out of 784 participants, 296 relapsed patients reported decision-making times: 169 (57%) had ≤1 week, and 127 (43%) had >1 week. Participants averaged 66±9 years old; 52% female, 91% White, 5% Black, 6% Hispanic/Latino, and 46% held graduate degrees.
The cohort given < 1 week expressed less satisfaction with their level of involvement in the treatment decision-making process (4.0±0.9 v. 4.2±0.8, p< 0.05) and were less comfortable with their final treatment decision (4.2±0.8 v. 4.4±0.7, p< 0.05). However, when a change in therapy was decided, time did not have an effect on the number of patients who suggested a different treatment or modification (>1 week: 42% vs. ≤1 week: 44%). In addition, the cohort rated their high-risk status as more influential for their treatment decision (2.2±1.7 vs. 1.7±1.8, p< 0.05) and were more likely to have the doctor make the final treatment decision (54%, n=68 vs. 30%, n=50, p< 0.001).
The cohort given >1 week rated side effect severity as more influential at the first treatment change ( >1 week: 3.5±1.3 vs. ≤1 week: 3.1±1.2, p< 0.05), a higher understanding of: FDA-approved therapies (3.9±1.0 v. 3.6±1.1, p< 0.05), efficacy of treatments (3.8±0.9 v. 3.5±1.0, p< 0.05), and efficacy-side effects balance (3.8±0.9 v. 3.6±1.1, p< 0.05). They also rated their own research on myeloma more favorably (3.9±1 v. 3.5±1.1, p< 0.05).
Both groups utilized educational resources at similar rates, but those with >1 week reported a higher use of webinars (3.2±1.3 v. 2.9±1.3, p< 0.05). There was no difference in satisfaction with the level of education and familiarity with treatment options.
Conclusions:
Most patients have less than a week to make a treatment decision, which often leads them to defer to their doctor and feel influenced by their high-risk status. Patients given >1 week reported greater satisfaction, comfort, and understanding of therapies. This highlights the need for proactive treatment strategies, supporting the idea that “there is no just-in-time education or trust,” emphasizing the importance of being prepared for a myeloma relapse.
