Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Optimizing Belantamab Mafodotin Doses for the Treatment of Transplant-Ineligible Newly Diagnosed Multiple Myeloma in the DREAMM-9 study
(PA-416) Optimizing Belantamab Mafodotin Doses for the Treatment of Transplant-Ineligible Newly Diagnosed Multiple Myeloma in the DREAMM-9 study

Karthik Ramasamy, MBBS, FRCP, FRCPath, PhD
Professor
NDORMS, University of Oxford, Oxford, UK
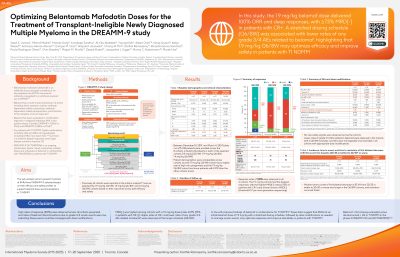
DREAMM-9 (NCT04091126), an ongoing randomized Phase 1 dose and schedule evaluation study, assessed belantamab mafodotin (belamaf) + bortezomib, lenalidomide, and dexamethasone (VRd) in autologous stem cell transplant (ASCT)-ineligible newly diagnosed multiple myeloma (TI NDMM). Early, deep anti-myeloma responses and no unexpected safety signals were reported for all cohorts.1 Here we report data on doses and schedules in 3 cohorts that support dose recommendations for TI NDMM.
Methods: Patients (pts) ≥18 years (yrs) ineligible for ASCT and with no prior MM treatment were dosed in cohorts with differing belamaf doses/schedules. All cohorts received belamaf and standard VRd for Cycles 1‒8 (21-day cycle), then Rd for Cycles 9+ (28-day cycle). Primary endpoint was safety/tolerability. Efficacy endpoints included overall response rate (ORR, % of pts with a confirmed partial response or better); complete response rate (CRR, % of pts with a complete response or better [ >CR]); and minimal residual disease negativity rate (MRD[-], % of pts with >CR and reached MRD negativity at 10-5 threshold by next-generation sequencing). Responses were assessed per International Myeloma Working Group criteria (2016).
Results:
As of Mar 4, 2024, a total of 108 pts were enrolled in 8 cohorts1: 12 pts were treated in each of the 1.9 mg/kg Q3/4W (1.9 SHORT), 1.9 mg/kg Q6/8W (1.9 STRETCH), and 1.4 mg/kg Q6/8W (1.4 STRETCH) cohorts. ORR % (CRR %) was 100 (75)/100 (92)/100 (91), respectively. Median time (months) to >VGPR was: 1.9 SHORT, 2.8; 1.9 STRETCH, 2.9; 1.4 STRETCH, 2.1. In pts with >CR, MRD[-] rates were 100% (n=9)/73% (n=8)/50% (n=5).
Of the pts who received ≥1 dose of belamaf, 67% (n=8)/25% (n=3)/33% (n=4) of pts in the 1.9 SHORT/1.9 STRETCH/1.4 STRETCH cohorts had Grade 3+ (Gr3+) belamaf-related AEs. Ocular exam findings (Gr3+) based on keratopathy and visual acuity scale were reported in 83% (n=10)/92% (n=11)/75% (n=9) of pts, respectively, comprising 26%/10%/18% of all assessments. AEs led to belamaf dose interruptions/delays in 83% (n=10)/75% (n=9)/83% (n=10). Belamaf dose reductions were seen in 42% (n=5)/83% (n=10)/42% (n=5) of affected pts.
Median (days) time to first bilateral decrease in BCVA to 20/50 or worse in pts with 20/25 or better in ≥1 eye at baseline was longer with Q6/8W schedules (1.9 STRETCH, 245.5; 1.4 STRETCH, 263.5) than Q3/4W (1.9 SHORT 76.0): these BCVA decreases resolved in a median of 1.4 STRETCH 70.0, 1.9 STRETCH 135.0, and 1.9 SHORT 163.0 days.
Conclusions:
Of the cohorts described the results indicate that belamaf + VRd induced deeper MRD[-] responses at the higher initial dose (1.9 mg/kg), with improved tolerability at the longer schedules (Q6/8W). In line with Terpos et al2, these data show that belamaf 1.9 mg/kg with an extended schedule achieved the positive benefit:risk ratio for the treatment of pts with TI NDMM.
1. Usmani et al. Blood, 2024
2. Terpos et al. Haematologica, 2024
Funding: GSK (209664).
