Imaging, QoL and Patient-Reported Outcome and Supportive Care
Category: Imaging, QoL and Patient-Reported Outcome and Supportive Care
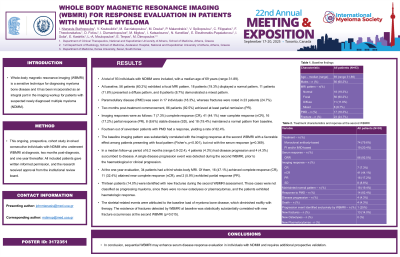
Whole Body Magnetic Resonance Imaging (WBMRI) for Response Evaluation in Patients with Multiple Myeloma
(PA-144) Whole Body Magnetic Resonance Imaging (WBMRI) for Response Evaluation in Patients with Multiple Myeloma

Ioannis Ntanasis-Stathopoulos, MD (he/him/his)
Clinical and research fellow
Department of Clinical Therapeutics, National and Kapodistrian University of Athens, School of Medicine, Athens, Greece
Whole-body magnetic resonance imaging (WBMRI) is a sensitive technique for diagnosing myeloma bone disease and it has been incorporated as an integral part in the imaging workup for patients with suspected newly diagnosed multiple myeloma (NDMM).
Methods:
This ongoing, prospective, cohort study involved consecutive individuals with NDMM who underwent WBMRI at diagnosis, two months post-diagnosis, and one year thereafter. All included patients gave written informed permission, and the research received approval from the institutional review board.
Results:
A total of 93 individuals with NDMM were included, with a median age of 69 years (range 31-89). At baseline, 56 patients (60.2%) exhibited a focal MRI pattern, 18 patients (19.3%) displayed a normal pattern, 11 patients (11.8%) presented a diffuse pattern, and 8 patients (8.7%) demonstrated a mixed pattern. Paramedullary disease (PMD) was seen in 17 individuals (18.3%), whereas fractures were noted in 23 patients (24.7%). Two months post-treatment commencement, 86 patients (92.5%) achieved at least partial remission (PR). Imaging responses were as follows: 7 (7.3%) complete response (CR), 41 (44.1%) near complete response (nCR), 16 (17.2%) partial response (PR), 8 (8.6%) stable disease (SD), and 18 (19.4%) maintained a normal pattern at baseline. Fourteen out of seventeen patients with PMD had a response, yielding a rate of 82.4%. The baseline imaging pattern was substantially correlated with the imaging response at the second WBMRI with a favorable effect among patients presenting with focal pattern (Fisher’s, p< 0.001), but not with the serum response (p=0.369).
In a median follow-up period of 6.2 months (range 0.9-22.4), 4 patients (4.3%) had disease progression and 4 (4.3%) succumbed to disease. A single disease progression event was detected during the second WBMRI, prior to the haematological or clinical progression. At the one-year evaluation, 34 patients had a third whole-body MRI. Of them, 16 (47.1%) achieved complete response (CR), 11 (32.4%) attained near complete response (nCR), and 2 (5.9%) exhibited partial response (PR).
Thirteen patients (14.0%) were identified with new fractures during the second WBMRI assessment. Those cases were not classified as progressing myeloma, since there were no new osteolyses or plasmacytomas, and the patients exhibited haematologic response. The skeletal-related events were attributed to the baseline load of myeloma bone disease, which diminished swiftly with therapy. The existence of fractures detected by WBMRI at baseline was statistically substantially correlated with new fracture occurrences at the second WBMRI (p=0.015).
Conclusions:
In conclusion, sequential WBMRI may enhance serum disease response evaluation in individuals with NDMM and requires additional prospective validation.
