Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
Differential impact of BCMA (TNFRSF17) extracellular domain mutations on in vitro potency of elranatamab versus teclistamab
(PA-039) Differential Impact of BCMA (TNFRSF17) Extracellular Domain Mutations on in vitro Potency of Elranatamab versus Teclistamab
- MJ
Maria Josic, MS
Principal Scientist
Pfizer
Introduction:
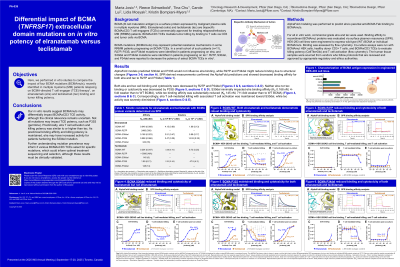
BCMA (B cell maturation antigen) is a surface protein expressed by malignant plasma cells in multiple myeloma (MM). Elranatamab (elra) and teclistamab (tec) are bispecific BCMAxCD3 T cell engagers (TCEs) commercially approved for treating relapsed/refractory MM (RRMM) patients. BCMAxCD3 TCEs mediate tumor killing by binding to T cells via CD3 and tumor cells via BCMA.
BCMA mutations (BCMAmuts) may represent potential resistance mechanisms in some RRMM patients progressing on BCMA TCEs. In a small cohort of such patients (n=11), R27P, P33S, and P34del mutations were identified in patients progressing on elra, and S30del and P34del mutations were identified in patients progressing on tec (Lee et al, 2023). R27P, S30del, and P34del were reported to decrease the potency of select BCMA TCEs in vitro.
Here, we performed in vitro studies to compare the impact of these BCMAmuts on elra and tec binding and tumor killing potency.
Methods: AlphaFold modeling was performed to predict elra’s parental anti-BCMA Fab binding to BCMAmuts. For all in vitro work, commercial grade elra and tec were used. Binding affinity to recombinant BCMAmut proteins was evaluated via surface plasmon resonance (SPR). HEK-293 cell lines were engineered to express wild type (WT) BCMA or individual BCMAmuts. Binding was assessed by flow cytometry. Co-culture assays were run with BCMAmut HEK cells, healthy donor CD3+ T cells, and BCMAxCD3 TCEs to evaluate killing potency (CellTiterGlo) and T cell activation (flow cytometry).
Results:
AlphaFold models predicted S30del and P33S would not influence elra binding, while R27P and P34del might reduce binding due to structural changes. SPR-derived measurements confirmed the AlphaFold predictions and showed decreased binding affinity for both elra and tec to R27P and P34del. Both elra and tec cell binding and cytotoxicity were decreased by R27P and P34del. Neither elra nor tec binding or cytotoxicity was decreased by P33S. S30del minimally impacted elra binding affinity (KD 0.168 nM, 4-fold weaker than to WT BCMA), while tec binding affinity was substantially reduced (KD 145 nM, 711-fold weaker than to WT BCMA). Correspondingly, elra T cell mediated killing with associated T cell activation was maintained toward S30del, while tec activity was severely diminished.
Conclusions:
These in vitro results suggest BCMAmuts may differentially impact BCMAxCD3 TCE activity, although the clinical relevance remains uncertain. Not all mutations may impact TCE potency, such as P33S (germline). Preclinically, elra T cell activation and killing potency was similar to or higher than tec. As preclinical binding affinity and killing potency is maintained, elra may have increased activity for patients harboring the S30del mutation. Further understanding mutation prevalence may inform if various BCMAxCD3 TCEs select for specific mutations, which could inform optimal treatment sequencing and selection, although these results must be clinically validated.
