Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Real-World Use of Melflufen plus Dexametasone in Relapsed/Refractory Multiple Myeloma: A Retrospective Study from the Valencian Community and the Region of Murcia (Spain)
(PA-493) Real-World Use of Melflufen plus Dexametasone in Relapsed/Refractory Multiple Myeloma: A Retrospective Study from the Valencian Community and the Region of Murcia (Spain)

Javier de la Rubia, Prof. Dr. (he/him/his)
Head of Department
Hematology Department, University Hospital La Fe
Melphalan fluflenamide (melflufen) in combination with dexamethasone (Melf-dex) has recently been approved in patients with relapsed/refractory multiple myeloma (RRMM) after ≥3 prior lines of therapy. However, real-world evidence remains limited to small cohorts, and data on patients pre-treated with T-cell engagers (TCEs) or CAR-T cell therapy are lacking. Here, we report data from a larger real-world cohort, including patients exposed to novel immunotherapies- a population not previously studied.
Methods:
Data were retrospectively collected from patients with RRMM who were treated with Melf-dex in the real-world setting from June 2024 to May 2025, at 9 institutions in Valencia and Murcia (Spain). Clinical and biological baseline characteristics, as well as information on treatment efficacy and safety were collected from medical records. Data analysis was performed using Microsoft Excel and R software. The study was approved by the Ethics Committee of the coordinating center.
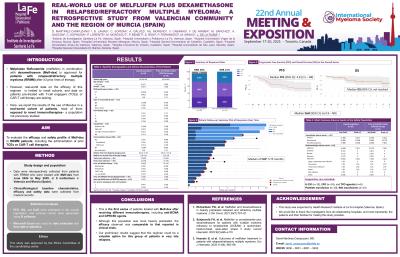
Results:
A total of 19 patients were included in the cohort. At study entry, the median age was 64 years, with a median of five prior lines of therapy. Seven patients (39%) presented with extramedullary disease, and six (35%) had high-risk cytogenetics, including four with ≥2 high-risk abnormalities. Eighteen patients (95%) were triple-class refractory and 14 (74%) were penta-class refractory. A total of 14 of patients (74%) had previously received some anti-BCMA and/or anti-GPRC5D therapy, including four cases of dual exposure. An overall response rate of 26% (n=5) was observed in the total cohort, compared to 23% (n=3) in the immunotherapy-exposed subgroup. Rates of stable disease were 42% and 38%, respectively. The median progression-free survival was 4.8 months (95% CI: 2.5-not reached), while at a median follow-up of 5.75 months the median overall survival had not been reached. Three patients remain alive and in response after over nine months of Melf-dex initiation. Grade III/IV hematologic toxicities were observed in 89% of patients, most commonly thrombocytopenia (68%), neutropenia (68%) and anemia (47%). Supportive care included G-CSF (n=15), EPO (n=14), TPO agonists (n=6), and platelet and red blood cell transfusions (n=10 and n=13, respectively). Infections were reported in 10 patients (53%), including three ≥ grade III cases. One patient permanently discontinued the regimen due to severe thrombocytopenia and bleeding, and another died of sepsis.
Conclusions:
This is the first real-world report on the use of Melf-dex in a cohort of patients previously exposed to anti-BCMA and anti-GPRC5D therapies. Although this population was more heavily pretreated, the efficacy observed was comparable to that reported in clinical trials. These findings suggest that Melf-dex may represent a valuable treatment option in this challenging setting. Longer follow-up and larger cohorts are needed to refine these preliminary results and establish the therapeutic role of this regimen in patients with advanced RRMM.
