Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
Effectiveness, safety and clinical use of teclistamab in patients with triple-class-exposed multiple myeloma. Data from the Danish ABC-study.
(PA-036) Effectiveness, Safety and Clinical Use of Teclistamab in Patients with Triple-class-exposed Multiple Myeloma. Data from the Danish ABC-study

Astrid Hundebøll Torpe (she/her/hers)
MD, hematologist in training.
Copenhagen University Hospital, Rigshospitalet, Department of Hematology
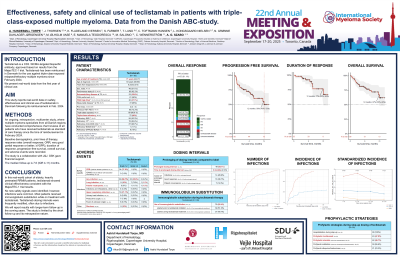
This study reports the real-world effectiveness, safety, and clinical use of teclistamab in Denmark following its reimbursement in February 2024 as standard of care (SOC) for triple-class-exposed (TCE) relapsed/refractory multiple myeloma (RRMM). Teclistamab is a BCMA-targeted bispecific antibody (BsAb), approved based on the MajesTEC-1 trial. We present real-world data from the first year of clinical use.
Methods:
In this ongoing, retrospective, multicenter study, myeloma specialists from all Danish healthcare regions reviewed patient charts of all TCE RRMM patients treated with SOC teclistamab during its first year of availability. Data collected included baseline demographics, prior lines of therapy (pLOT), response rates, progression-free survival (PFS), duration of response (DOR), overall survival (OS), adverse events (AEs), and clinical use patterns. The study was conducted in collaboration with Johnson & Johnson and GSK provided financial support.
Results:
Ninety patients received teclistamab between February 2024 and February 2025. Median follow-up was 8 (IQR 4-11) months. Median age at treatment initiation (T0) was 71 years; 51% were male. Median number of pLOT was 4, and median time since diagnosis was 6 years.
High-risk FISH [t(4;14), t(14;16), or del17p] was present in 37% of patients. Performance status was 0-1 in 92%, and 26% had extramedullary disease.
Most patients (99%) were TCE; 80% were triple-class refractory; 10% were refractory to GPRC5D BsAbs, and 72% had undergone autologous transplant.
Overall response rate (ORR) was 61%, with 54% of patients achieving ≥VGPR. Fourteen percent had unmeasurable disease at T0 and were not evaluable for response.
Median PFS was not reached; at 12 months 56% remained progression-free. Estimated 12-month DOR and OS were 77% and 67%, respectively.
All patients were hospitalized for step-up dosing, and 48% were treated with one dose of prophylactic tocilizumab during teclistamab step-up. Eighty-five percent of patients received immunoglobulin substitution while on treatment with teclistamab.
Most frequent AEs were cytokine release syndrome (CRS; 38% grade 1-2, none ≥grade 3) and infections. Sixty percent experienced infections; 25% were ≥ grade 3, including two grade 5 infections. Most common infections were upper respiratory and pulmonary.
Dosing intervals were extended in 55% of patients, deviating from the labeled regimen, after a median of 3 months. The most common extension was dosing every two weeks, with 29% of cases attributed to infections.
Conclusions:
In this real-world cohort of elderly, heavily pretreated RRMM patients, teclistamab showed clinical effectiveness consistent with MajesTEC-1. No new safety signals were identified; however, infections were common. Most patients received immunoglobulin substitution while on treatment with teclistamab. Teclistamab dosing intervals were frequently modified, often due to infections.
