Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
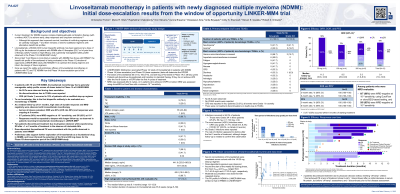
Linvoseltamab (LINVO) monotherapy in patients (pts) with newly diagnosed (ND) multiple myeloma (MM): Initial dose-escalation results from the window of opportunity LINKER-MM4 trial
(PA-027) Linvoseltamab (LINVO) Monotherapy in Patients (pts) with Newly Diagnosed (ND) Multiple Myeloma (MM): Initial Dose-escalation Results from the Window of Opportunity LINKER-MM4 Trial
Christopher J. Ferreri, MD
Assistant Professor
Atrium Health Levine Cancer Institute, Wake Forest University School of Medicine, Charlotte, NC, USA
LINVO, a B-cell maturation antigen (BCMA)×CD3 bispecific antibody, achieved an overall response rate (ORR) of 71% (complete response [CR] or better [≥CR] 52%) at the 200 mg dose in pts with relapsed/refractory (RR) MM. Pts with NDMM are likely to have more intact T-cell fitness than pts with RRMM, supporting study of LINVO in NDMM. We report safety and preliminary efficacy of LINVO monotherapy dose escalation in pts with NDMM in the open-label Phase (Ph) 1/2 LINKER-MM4 study (NCT05828511).
Methods:
Adults with previously untreated, symptomatic MM who were autologous stem cell transplantation (ASCT) eligible (TE) or ineligible (TIE) were enrolled. TE pts received LINVO induction then ASCT and LINVO consolidation; TIE pts received LINVO monotherapy until disease progression. Initial dose-escalation (Ph1A) and -expansion (Ph1B) data will inform the recommended Ph2 dose. Ph1A included modified step-up dosing (1 mg on Cycle [C] 1 Day [D] 1, 4 mg on C1D4, 25 mg on C1D8) and evaluated three full doses (50, 100, 200 mg). Ph1 primary endpoints were incidences of dose-limiting toxicities (DLTs), treatment-emergent AEs (TEAEs) and AEs of special interest. Secondary endpoints included ORR and depth of response by International Myeloma Working Group criteria, duration of response (DOR), and progression-free survival (PFS).
Results:
By Feb 11, 2025, 12 pts had received LINVO (50 mg, n=3; 100 mg, n=4; 200 mg, n=5) in Ph1A; 75% were TE. Median follow-up was 9.1 months (mo; range 1.6–12.9). Median age was 64.5 years (range 43–82); 67% were male, 50% White, 42% Black/African American; 67% had bone marrow plasmacytosis ≥50%, 8% extramedullary plasmacytomas, 50% sBCMA ≥400 ng/mL, 42% R-ISS II, and 50% high cytogenetic risk.
No DLTs were observed. Among all pts, the most common TEAEs were increased alanine aminotransferase (any Grade [Gr], 67%; Gr 3–4, 17%) and aspartate aminotransferase (50%; all Gr 1–2; transient in all but one pt). The most common hematologic TEAE was neutropenia (50%; all Gr 3–4). CRS was reported in 33% of pts (all Gr 1). No ICANS events were reported. Infections occurred in 58% of pts (Gr 3–4, 25%). There were no treatment discontinuations due to TEAEs or TEAEs resulting in death.
Investigator-assessed ORR was 83%; 75% achieved ≥VGPR and 58% ≥CR. Median time to response was 1.1 mo. Five of seven CRs occurred within 6 mo of treatment initiation. Five pts (200 mg, n=3; 100 mg, n=2) were MRD evaluable, and all were MRD negative at 10−6 by clonoSEQ. Median DOR and PFS were not reached. At 6 mo, all pts maintained their response and were progression free. LINVO pharmacokinetics in NDMM aligned with prior RRMM findings.
Conclusions:
LINVO monotherapy had a generally manageable safety profile across all doses tested in TE and TIE pts with NDMM. The ORR, CR rate, MRD-negativity rate, and response durability were promising, supporting ongoing assessment of LINVO monotherapy in the front-line setting.
