Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
Real-World Long-Term Effectiveness and Safety Outcomes Among Patients Receiving Teclistamab for the Treatment of Relapsed/Refractory Multiple Myeloma (RRMM)
(PA-022) Real-World Long-Term Effectiveness and Safety Outcomes Among Patients Receiving Teclistamab for the Treatment of Relapsed/Refractory Multiple Myeloma (RRMM)

Carlyn Rose Tan, MD (she/her/hers)
Assistant Attending Physician, Myeloma Service
Memorial Sloan Kettering Cancer Center
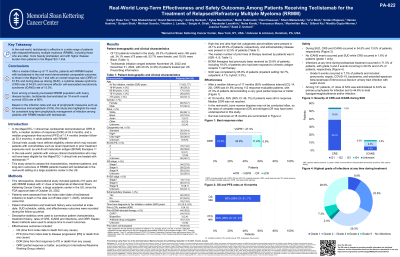
In the MajesTEC-1 clinical trial, teclistamab (Tec) demonstrated an overall response rate (ORR) of 63% (median follow-up 30.4 months) in adult patients (pts) with RRMM. Pts in clinical trials may not fully reflect real-world (RW) pt populations, including pts with no prior anti-BCMA targeted therapy exposure. RW studies of Tec report ORRs of 59% to 66%, but many are limited by short follow-up periods. To address this evidence gap, this study aimed to assess long-term outcomes of pts treated with Tec in a RW setting.
Methods:
This retrospective observational study included adult pts with RRMM treated with ≥1 dose of Tec from October 2022 (FDA approval) to March 2025 at a large academic center in the US (cut-off date of April 1, 2025). Pts were assessed from the index date (date of Tec initiation) to death or the end of data cut off, whichever came first. Pt characteristics (frequency (%) or median) and treatment history were recorded at the index date. Dosing schedule and safety and effectiveness outcomes (IMWG criteria) were recorded during the follow-up period. Progression-free survival (PFS) and overall survival (OS) were reported (Kaplan Meier).
Results:
Of 123 pts included in the study, the median age was 71 years, 34.3% were ≥75 years old, 53.6% were female, and 19.5% were Black. High-risk cytogenetic abnormalities (including 1q+, del(17p), t(4;14), t(14;16), and t(14;20)) was present in 49.1% of pts. Pts had a median of 5 (range: 3-19) prior lines of therapy, 35.8% were BCMA-exposed (20.0% CAR-T, 2.5% bispecifics, 13.0% antibody-drug conjugates), 32.5% had extramedullary disease and 61.8% had received a stem cell transplant. After a median follow-up of 17 months (95% confidence interval: 14-20), ORR was 61.6% among 112 response-evaluable pts (47.3% had a best response of very good partial response or better). After 18 months of initiating Tec, response was maintained by 59% of pts. The 18-month PFS and OS rates were 36% and 60%, respectively. Step-up dosing (SUD) was completed by 95.9% of pts, with most (92.7%) administered in an inpatient setting (outpatient: 4.1%, hybrid: 3.3%). During SUD, cytokine release syndrome occurred in 54.5% of pts (all grade (G) 1/2) with 9.8% of pts experiencing an event after the first full dose. Immune effector cell-associated neurotoxicity syndrome occurred in 13.0% of pts (G1/2, except for one G4 event); 5.7% of pts experienced an event after the first full dose. Infections at any time during Tec treatment occurred in 71.5% of pts (G1: 8.9%, G2: 23.6%, G3: 29.3%, G4: 2.4%, G5: 7.3%). Among 121 pts, ≥1 dose of intravenous immunoglobin was administered to 6.5% as primary prophylaxis and to 44.6% to treat hypogammaglobulinemia and/or infection.
Conclusions:
Pts treated with Tec in the RW had comparable long-term effectiveness and safety outcomes to the MajesTEC-1 trial pts, despite pts in this analysis being older, more heavily pre-treated (including prior BCMA exposure), with more pts having high burden of disease and high-risk cytogenetics.
