Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Updated Results From the Phase 3 DREAMM-8 Study of Belantamab Mafodotin Plus Pomalidomide and Dexamethasone vs Pomalidomide Plus Bortezomib and Dexamethasone in Relapsed/Refractory Multiple Myeloma
(PA-469) Updated Results From the Phase 3 DREAMM-8 Study of Belantamab Mafodotin Plus Pomalidomide and Dexamethasone vs Pomalidomide Plus Bortezomib and Dexamethasone in Relapsed/Refractory Multiple Myeloma

Meletios A. Dimopoulos
Professor and Chairman of the Department of Clinical Therapeutics
National and Kapodistrian University of Athens, Athens, Greece
Methods:
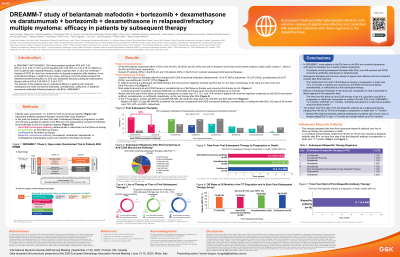
DREAMM-8 is a phase 3, open-label, randomized, multicenter trial evaluating the efficacy and safety of BPd vs PVd in pts with RRMM who received ≥1 prior LOT, including lenalidomide. Pts were randomized 1:1 to BPd (28-day cycles), which comprised belantamab mafodotin 2.5 mg/kg IV (C1 D1), then 1.9 mg/kg (C2+ D1), plus pomalidomide 4 mg (D1-21, all cycles) and dexamethasone 40 mg (D1, QW, all cycles), or PVd (21-day cycles), which comprised pomalidomide 4 mg (D1-14, all cycles) plus bortezomib 1.3 mg/m2 SC (C1-8 D1, 4, 8, and 11; C9+ D1 and D8) and dexamethasone 20 mg (day of and 1 day after bortezomib dose). Treatment continued until progressive disease, unacceptable toxicity, or death. Efficacy assessments occurred Q4W.
Results: In the intention-to-treat population, 302 pts were randomized 1:1 to receive BPd (n=155) or PVd (n=147). At data cutoff (October 7, 2024), median follow-up was 28.01 mo (range, 0.03-47.74 mo); 55 pts (35%) in the BPd arm and 20 (14%) in the PVd arm had treatment ongoing. In the BPd arm, 68 pts (44%) experienced a PFS event as did 89 (61%) in the PVd arm. PFS benefit was maintained and favored BPd. Median PFS was 32.6 mo (95% CI, 21.1 mo-not reached) with BPd vs 12.5 mo (95% CI, 9.1-17.6 mo) with PVd (HR, 0.49; 95% CI, 0.35-0.68). The estimated 18-month PFS rate was 63% (95% CI, 54%-70%) with BPd vs 41% (95% CI, 32%-50%) with PVd. PFS benefit was maintained across subgroups, including pts with high-risk cytogenetics (unadjusted HR, 0.55; 95% CI, 0.33-0.90), lenalidomide-refractory disease (unadjusted HR, 0.43; 95% CI, 0.30-0.60), anti-CD38–refractory disease (unadjusted HR, 0.64; 95% CI, 0.36-1.15), 1 prior LOT (unadjusted HR, 0.47; 95% CI, 0.29-0.77), and ≥2 prior LOTs (unadjusted HR, 0.51; 95% CI, 0.33-0.77). Updated safety results were consistent with the primary analysis as presented previously and did not change the safety profile of BPd.
Conclusions: In DREAMM-8, BPd continued to demonstrate a clinically meaningful PFS benefit vs PVd in pts with RRMM with ≥1 prior LOT. This benefit was maintained across key subgroups, including pts with anti-CD38–and lenalidomide-refractory disease. No new safety signals were observed. These data further support BPd as a potential standard-of-care option in pts with RRMM.
Funding: GSK. Drug-linker technology licensed from Seagen Inc; monoclonal antibody produced using POTELLIGENT Technology licensed from BioWa.
