Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
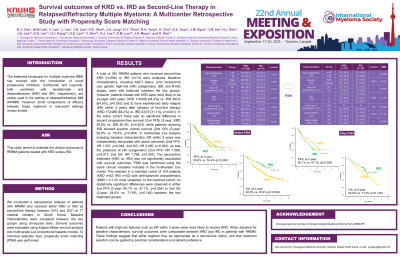
Survival outcomes of KRD vs. IRD as Second-Line Therapy in Relapsed/Refractory Multiple Myeloma: A Multicenter Retrospective Study with Propensity Score Matching
(PA-466) Survival outcomes of KRD vs. IRD as Second-Line Therapy in Relapsed/Refractory Multiple Myeloma: A Multicenter Retrospective Study with Propensity Score Matching

Hee jeong Cho (she/her/hers)
Assistant professor
Kyungpook National University Hospital
Introduction:
The treatment landscape for multiple myeloma (MM) has evolved with the introduction of novel proteasome inhibitors. Carfilzomib and ixazomib, both combined with lenalidomide and dexamethasone (KRD and IRD, respectively), are widely used in the setting of relapsed/refractory MM (RRMM). However, direct comparisons of efficacy between these regimens in real-world settings remain limited. This study aimed to evaluate the clinical outcomes of RRMM patients treated with KRD versus IRD.
Methods:
We conducted a retrospective analysis of patients with RRMM who received either KRD or IRD as second-line therapy between 2015 and 2021 at 17 medical centers in South Korea. Baseline characteristics were compared between the two groups using chi-square tests. Survival outcomes were evaluated using Kaplan–Meier survival analysis and multivariate Cox proportional hazards models. To minimize selection bias, propensity score matching (PSM) was performed.
Results: A total of 342 RRMM patients who received second-line KRD (n=268) or IRD (n=74) were analyzed. Baseline characteristics, including ASCT status, prior bortezomib use, gender, high-risk (HR) cytogenetics, ISS, and R-ISS stages, were well balanced between the two groups. However, patients treated with KRD were more likely to be younger (≤65 years: KRD 119/268 [44.4%] vs. IRD 48/74 [64.9%], p=0.002) and to have experienced early relapse (ER) within 2 years after initiation of front-line therapy (KRD 172/268 [64.2%] vs. IRD 23/74 [31.1%], p< 0.001). In the entire cohort, there was no significant difference in second progression-free survival (2nd PFS) (2-year: KRD 59.6% vs. IRD 50.4%, p=0.254), while patients receiving IRD showed superior overall survival (2nd OS) (2-year: 78.4% vs. 62.8%, p=0.004). In multivariate Cox analysis including baseline characteristics, ER within 2 years was independently associated with worse outcomes (2nd PFS: HR 1.531, p=0.044; 2nd OS: HR 2.050, p=0.003), as was the presence of HR cytogenetics (2nd PFS: HR 1.589, p=0.017; 2nd OS: HR 1.798, p=0.003). The second-line treatment (KRD vs. IRD) was not significantly associated with survival outcomes. PSM was performed using the same clinical variables included in the multivariate Cox model. This resulted in a matched cohort of 104 patients (KRD n=52; IRD n=52) with well-balanced characteristics (SMD < 0.1 for most variables). In the matched cohort, no statistically significant differences were observed in either 2nd PFS (2-year: 60.1% vs. 47.1%, p=0.254) or 2nd OS (2-year: 64.0% vs. 71.9%, p=0.148) between the two treatment groups.
Conclusions:
Patients with high-risk features such as ER within 2-years were more likely to receive KRD. When adjusted for baseline characteristics, survival outcomes were comparable between KRD and IRD in patients with RRMM. These findings suggest that either regimen may be appropriate as a second-line option, and that treatment selection can be guided by practical considerations and patient preference.
