Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
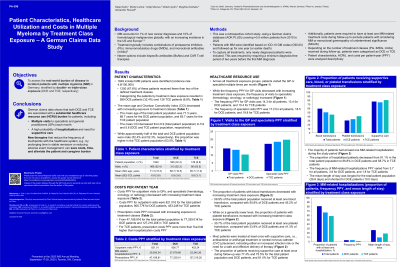
Patient Characteristics, Healthcare Utilization and Costs in Multiple Myeloma by Treatment Class Exposure – A German Claims Data Study
(PA-396) Patient Characteristics, Healthcare Utilization and Costs in Multiple Myeloma by Treatment Class Exposure – A German Claims Data Study
Alexander Russell, MSc (he/him/his)
Senior Director
Pfizer
Introduction:
Multiple myeloma (MM) accounts for 1% of new cancer diagnoses and 10% of hematological malignancies globally, with an increasing incidence in the US and Europe (Firth 2019; Padala 2021). Treatment typically includes combinations of protease inhibitors (PIs), immunomodulatory drugs (IMIDs), and monoclonal antibodies (mAbs) (Rajkumar 2022). Newer options include bispecific antibodies (BsAbs) and CAR-Ts. This study assessed the real-world burden of disease in incident patients (pts) with MM in Germany, stratified by double- vs. triple-class exposure (DCE-TCE, respectively).
Methods:
Our retrospective cohort study used claims data from AOK PLUS, a German sickness fund covering about 3.5 million pts from 2010-2022; this is prior to the recent novel monotherapy era, so does not capture BsAbs. We included incident pts with a first MM diagnosis (ICD-10-GM: C90.00) between 2012-2022, excluding those with a MM diagnosis within the previous 24-months. Patients were observed during follow-up, for one year or until death, and depending on the number of treatment classes (PIs, IMIDs, or mAbs incl. anti-CD38) were stratified into DCE and TCE. Pts were censored in the DCE group when entering the TCE group. Pts without any of these treatment classes were excluded. We descriptively analyzed pt baseline characteristics, as well as healthcare resource utilization (HCRU) and costs per patient-year (PPY).
Results:
We identified 1849 incident MM pts (male: 52.4%; mean age: 71.3 yr; mean Charlson Comorbidity Index [CCI]: 6.9), resulting in an incidence rate of 4.8/100,000. Of these, 599 pts (32.4%) were categorized as DCE and 126 pts (6.8%) were categorized as TCE. Compared with DCE pts, TCE pts were younger (mean age: 68.7 vs 65.7yr), more often male (52.3% vs 63.5%), and had a slightly lower CCI (mean CCI: 5.9 vs 5.6). Although more DCE pts had MM-related hospitalizations vs TCE pts (66.8% vs 58.7%), their mean length of stay was shorter (10.0 vs 18.9d PPY). DCE pts had more visits to the GP (13.4 vs 10.4 PPY) but fewer visits to specialists (hematology, oncology, or radiology; 18.5 vs 19.8 PPY) than TCE pts. Blood and platelet transfusions were given to 50.8% and 33.9% (DCE) or 45.2% and 41.3% (TCE) of pts, respectively. Supportive care was administered to 75.5% of DCE and 81.0% of TCE pts. Prescriptions (DCE: 77,329€, 56.1%; TCE: 127,216€, 71.1%) and MM-related hospitalizations (DCE: 37,680€, 27.3%; TCE: 23,345€, 13.1%) had the highest cost PPY.
Conclusions: Outpatient data in Germany shows that both DCE and TCE MM is associated with a substantial HCRU burden for pts. Pts visit their specialists and GPs multiple times each month; the probability of hospitalization and need for supportive care is high. New therapies that reduce the frequency of touchpoints with the healthcare system, e.g. by prolonging time in stable remission or reducing adverse event management, will save costs, time, and alleviate the pt and caregiver burden.
