Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Impact of CD34+ Cell Infusion Dose on Immune reconstitution and Survival in Multiple Myeloma after Autologous Stem Cell Transplantation
(PA-384) Impact of CD34+ Cell Infusion Dose on Immune Reconstitution and Survival in Multiple Myeloma After Autologous Stem Cell Transplantation

Lijuan Chen, MD
professor
Department of Hematology, The First Affiliated Hospital with Nanjing Medical University
Introduction:
Autologous stem cell transplantation (ASCT) remains a cornerstone therapy for multiple myeloma (MM). However, the optimal CD34+ cell infusion dose and its relationship with immune reconstitution and survival are unclear. Oligoclonal bands (OB), indicating B-cell recovery, may serve as markers of effective immune reconstitution. This study aimed to evaluate the prognostic impact of CD34+ cell infusion dose and to explore its association with OB formation, in order to inform transplant optimization.
Methods:
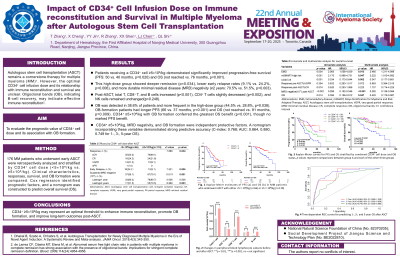
A total of 176 MM patients who underwent early ASCT were retrospectively analyzed and stratified by CD34+ cell dose (< 5×10⁶/kg vs. ≥5×10⁶/kg). Clinical characteristics, treatment responses, survival outcomes, and OB formation were compared. Prognostic factors were identified via Cox regression, and a nomogram was constructed to predict overall survival (OS).
Results:
Patients receiving a CD34+ cell infusion ≥5×10⁶/kg demonstrated significantly improved progression-free survival (PFS: 50 vs. 40 months, p=0.020) and OS (not reached vs. 76 months, p< 0.001) compared to those receiving < 5×10⁶/kg. This high-dose group also showed deeper remission (p=0.034), lower early relapse rates (9.1% vs. 24.2%, p=0.006), and more durable minimal residual disease (MRD) negativity (≥2 years: 70.5% vs. 51.5%, p=0.003). Immune reconstitution analysis revealed significant increases in total T cells, CD8+ T cells, and B cells post-ASCT (p< 0.001), alongside a modest reduction in CD4+ T cells (p=0.002) and no significant change in NK cells (p=0.248). OB was detected in 38.6% of patients and was significantly associated with high CD34+ dose (44.5% vs. 28.8%, p=0.038). OB-formation patients exhibited longer PFS (66 vs. 37 months, p< 0.001) and OS (not reached vs. 91 months, p=0.009). Combined analysis revealed that CD34+ ≥5×10⁶/kg with OB formation conferred the greatest OS benefit (p< 0.001), though no marked PFS benefit. CD34+ ≥5×10⁶/kg, MRD negativity, and OB formation were independent protective factors. A nomogram incorporating these variables demonstrated strong predictive accuracy (C-index: 0.768; AUC: 0.864, 0.880, 0.749 for 1-, 3-, 5-year OS) , supporting its clinical utility.
Conclusions:
This study identifies CD34+ ≥5×10⁶/kg infusion as a potential optimal threshold that enhances immune reconstitution and promotes OB formation, thereby improving deep remission and long-term survival after ASCT.
