Myeloma Novel Drug Targets and agents
Category: Myeloma Novel Drug Targets and agents
Carfilzomib, pomalidomide, dexamethasone±daratumumab delivers survival benefit regardless of cytogenetic risk in early relapsed myeloma patients:a multi-center, prospective real world study in China
(PA-327) Carfilzomib, Pomalidomide, Dexamethasone±daratumumab Delivers Survival Benefit Regardless of Cytogenetic Risk in Early Relapsed Myeloma Patients:a Multi-center, Prospective Real World Study in China

Fujing Zhang, MD Candidate (she/her/hers)
MD Candidate
Department of Hematology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing, China
This study aims to evaluate the efficacy and safety of carfilzomib, pomalidomide, and dexamethasone with or without daratumumab in treating relapsed/refractory multiple myeloma in real-world practice.
Methods:
This multicenter, prospective, real-world cohort study was conducted across eight hospitals in northern China since 2022. Eligible participants included adults diagnosed with RRMM who had received at least one prior line of therapy. Patients were treated with KPd with or without Dara until disease progression. Data on baseline characteristics, cytogenetic abnormalities, and adverse events were collected. Carfilzomib, pomalidomide, dexamethasone, (and Dara) were administered in 28-day cycles. The primary endpoint was the overall response rate (ORR), with secondary endpoints including progression-free survival (PFS) and overall survival (OS). Statistical analyses included χ²-test, t-test, Kaplan-Meier, and COX regression methods.
Results:
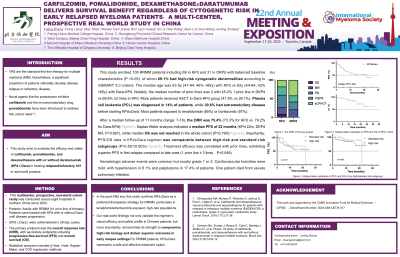
This study enrolled 100 RRMM patients including 69 in KPd and 31 in DKPd with balanced baseline characteristics (P >0.05), of whom 69.1% had high-risk cytogenetic abnormalities according to mSMART 3.0 criteria. The median age was 63.5y (47-84; 46% >65y) with KPd vs 62y (44-84; 42% >65y) with Dara-KPd. Notably, the median number of prior lines was 2 with 45.2% 1 prior line in DKPd vs 69.6% ≥2 lines in KPd. More patients received ASCT in Dara-KPd group (41.9% vs 26.1%). Plasma cell leukemia (PCL) was diagnosed in 14% of patients, while 30.6% had extramedullary disease before starting KPd±Dara. Most patients exposed to lenalidomide (85%) or bortezomib (97%).
After a median follow-up of 11 months (range: 7-18), the ORR was 75.4% (73.3% for KPd vs. 79.2% for Dara-KPd). Kaplan-Meier analysis indicated a median PFS of 22 months (KPd 22m, DKPd NR, P=0.687), while median OS was not reached in the whole cohort (P=0.790). Importantly, PFS/OS data in KPd±Dara regimen was comparable between high-risk and standard-risk subgroups (P=0.501/0.603). Treatment efficacy was correlated with prior lines, exhibiting superior PFS in first relapse compared to late ones (1 prior line ≥ 3 lines,P=0.049).
Hematologic adverse events were common but mostly grade 1 or 2. Cardiovascular toxicities were mild, with hypertension in 8.1% and palpitations in 17.4% of patients. One patient died from severe pulmonary infection.
Conclusions:
In the post-VRd era, this study confirms KPd±Dara as a preferred therapeutic strategy for RRMM, particularly in lenalidomide/bortezomib-exposed, high-risk populations.
Our real-world findings not only validate the regimen's robust efficacy and safety profile in Chinese patients, but more importantly, demonstrate its strength to compromise high-risk biology and deliver superior outcomes in early relapse settings.For RRMM patients, KPd±Dara represents a safe and effective treatment option.
